New easy-to-understand validations in clinical documentation help clinicians complete accurate, compliant and timely documentation.
Automated quality assurance checks occur in Axxess Hospice prior to reviewing clinical documentation through the agency’s QA process. This functionality streamlines operations and facilitates compliance through built-in review features that ensure documentation aligns with CMS regulations.
These enhancements fall into two main categories: Field Validations and Hospice Item Set Validations.
Throughout clinical documentation for each discipline, required fields are identified with red asterisks. When Save or Complete is selected, each required field is automatically checked for completion. If any information is missing, a warning message alerts the user to complete the missing information.
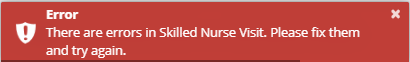
Items that are left blank or have incorrect information will be highlighted in red and a brief explanation of the error will be provided.
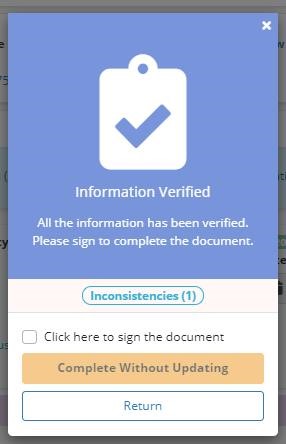
The software will automatically move to the next field that requires correction so that each item can be corrected before attempting to save or complete the document again. Once all necessary corrections have been made, a success message will appear on completion.
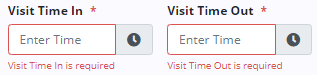
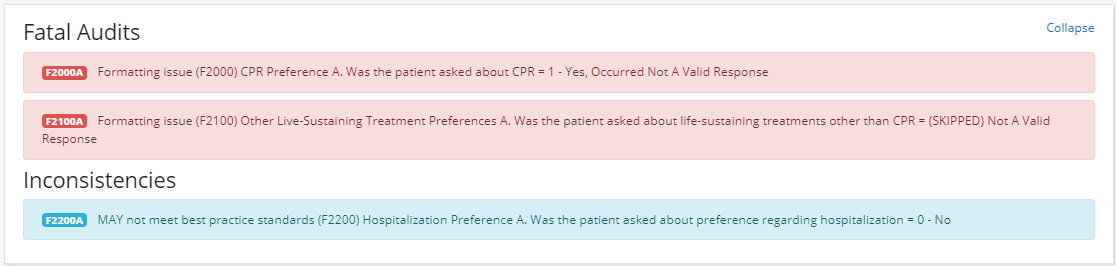
In addition to field validations, the software will also automatically run the HIS scrubber for the RN Initial/Comprehensive Assessment and RN Comprehensive Assessment when the Complete button is selected in these documents. Any errors, inconsistencies or warnings will display at the top of the assessment.
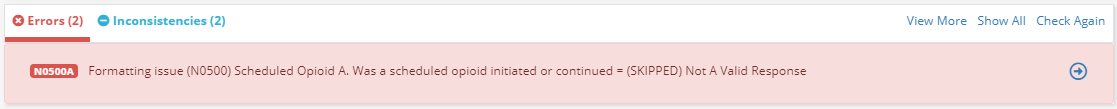
Use the arrow buttons to move between each error, inconsistency and/or warning. As you move through each message, the software will automatically move to the appropriate section and highlight the information that needs to be reviewed or corrected. Click Show All to view all errors, inconsistencies and warnings as a list. Click Collapse to close the list and return to the document.
Once all necessary corrections have been made, click Check Again to re-check the document by the HIS scrubber.
All errors must be corrected before the document can be completed to prevent the HIS data from being rejected by CMS. While all errors must be corrected, documents can be completed if inconsistencies and warnings remain.
The HIS scrubber can be run on demand at any time by clicking the Check Errors button at the bottom of the RN Initial/Comprehensive Assessment and RN Comprehensive Assessment.
Updated on 4/13/2020