The IDG Summary/Comprehensive Assessment Update enables Progress Toward Goals to flow automatically from each clinical document to the IDG Summary/Comprehensive Assessment. Instead of allocating time to writing IDG notes, clinicians can incorporate their routine visit documentation for each discipline into the Comprehensive Assessment automatically.
All changes to physician orders will automatically flow to the IDG Summary/Comprehensive Assessment, so the IDG team can review changes to the Plan of Care during IDG meetings. These include:
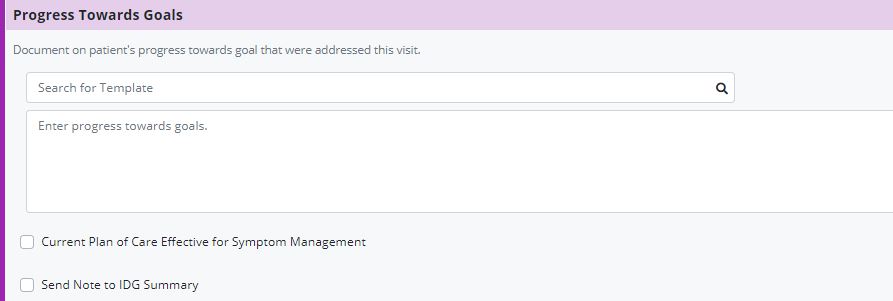
The Progress Toward Goals section of each clinical document enables clinicians to copy goals from the Plan of Care Profile and document the patient’s progress toward each goal.
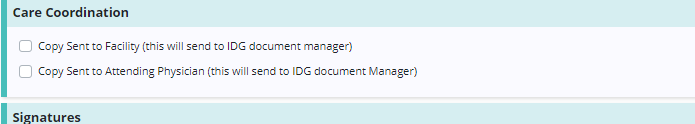
In some documents (including admission and recertification nursing assessments), the admission/recertification narrative and care coordination narrative documentation can be sent to the IDG Summary/Comprehensive Assessment Update.
If a clinician chooses not to check the Send Note to IDG Summary box, the IDG Summary/Comprehensive Assessment Update can be documented manually in the IDG Center. A user who has not had a visit with the patient in two weeks should update the IDG note manually in the IDG Center.
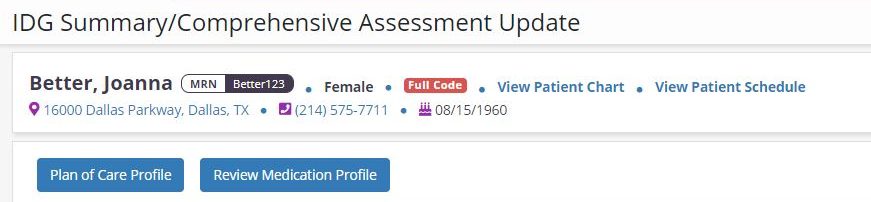
At the top of the IDG Summary/Comprehensive Assessment, blue buttons provide easy access to other parts of the patient’s chart before and after the IDG meeting. These buttons enable users to preserve work in the IDG note while viewing the Patient Chart, Medication Profile, Plan of Care, or adding a new physician order in a new tab.
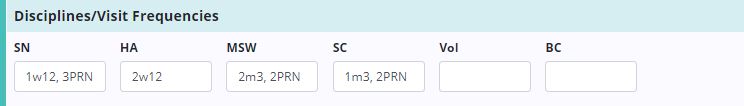
The visit frequencies for all ordered disciplines auto-populate from the most recent frequency orders.
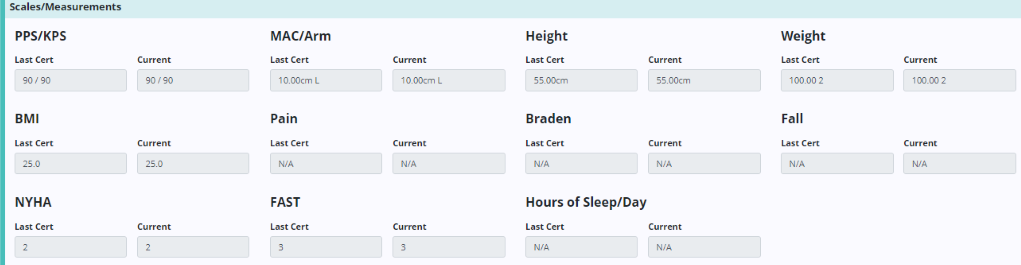
Scales and measurements automatically populate from the most recent certification assessment (RN Initial/Comprehensive Assessment or RN Recertification Assessment) for comparison to the most recent Skilled Nursing Visit. This data enables the IDG team to easily track declines in status throughout the benefit period.
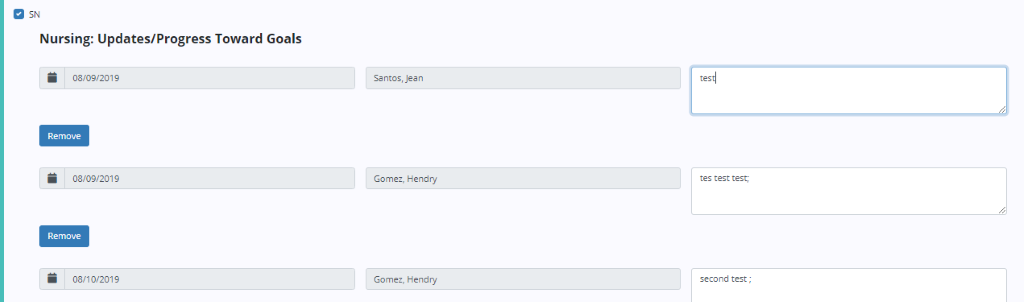
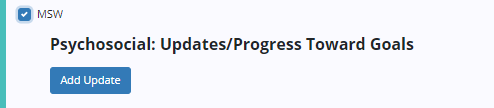
Updates and progress toward goals flow from the clinical documents into this section.
If the clinician selects Send Note to IDG:
The information will flow into this area with the date of the visit note and the clinician who documented the update. The update can be edited by the clinician who entered it, and new updates can be manually entered if necessary.
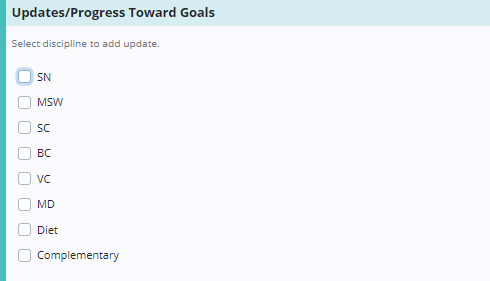
If the clinician does not select Send Note to IDG:
Users can select disciplines here to add notes manually.
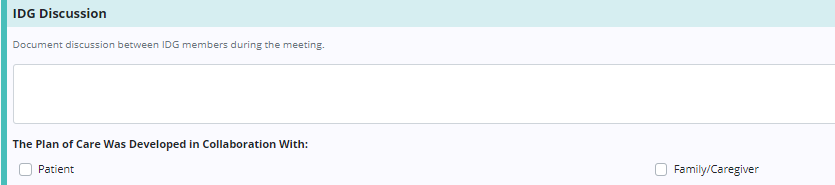
In the IDG Discussion section, users can document discussion during the IDG meeting. Any user who has joined the meeting can document in this section. Users can check Patient and/or Family/Caregiver to document their involvement in developing the Plan of Care as needed.
Care coordination between the hospice IDG, attending physician, and nursing care/residential facilities can be documented in the Care Coordination section.