Axxess Hospice now provides easy-to-use shift notes for patients receiving general inpatient and continuous care levels.
These shift notes enable organizations to easily accommodate the needs of patients receiving general inpatient or continuous care while staying compliant and providing seamless care delivery.
Due to the comprehensive nature of shift documentation and the many tools included in these notes, clinicians planning to use shift notes should have permission to view and manage the eMAR, Medication Profile and Patient Charts in Axxess Hospice.
To give a user the permissions needed to use shift documentation, edit the user’s profile and navigate to the Permissions tab.
People tab ➜ People Center ➜ Edit ➜ Permissions tab
In the Clinical section, select View, Add, Edit, Delete and Reassign next to the eMAR permission.
Clinical section ➜ eMAR ➜ View/Add/Edit/Delete/Reassign

Select View next to the Medication Profile permission.
Clinical section ➜ Medication Profile ➜ View
Select View and Edit next to the Patient Chart permission.
Clinical section ➜ Patient Chart ➜ View/Edit
Click Save to finish granting the permissions to the user.
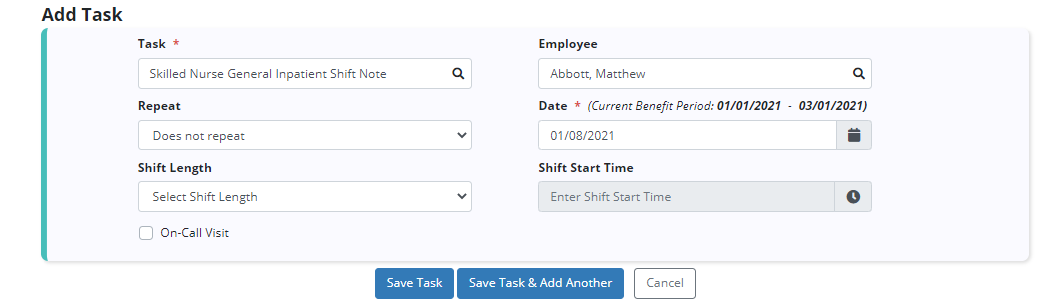
To schedule a Skilled Nurse General Inpatient Shift Note or Skilled Nurse Continuous Care Shift Note, navigate to the Patient Schedule or Employee Schedule under the Schedule tab.
Schedule tab ➜ Patient Schedule or Employee Schedule
Click Add Task. From the Task menu, select Skilled Nurse General Inpatient Shift Note or Skilled Nurse Continuous Care Shift Note.
Add Task ➜ Task menu ➜ Skilled Nurse General Inpatient Shift Note or Skilled Nurse Continuous Care Shift Note ➜ Save Task
These tasks are associated with the skilled nursing discipline frequency and will be calculated as part of the patient’s ordered frequency.
Once a task has been scheduled, users can complete the shift note by selecting the task on the Patient Schedule or Employee Schedule screen.
Shift notes are tabbed to enable users to focus on a particular body system or shift task.
The Administrative Information tab enables users to document details about the shift. Users are required to enter the visit date, shift start time and shift end time.
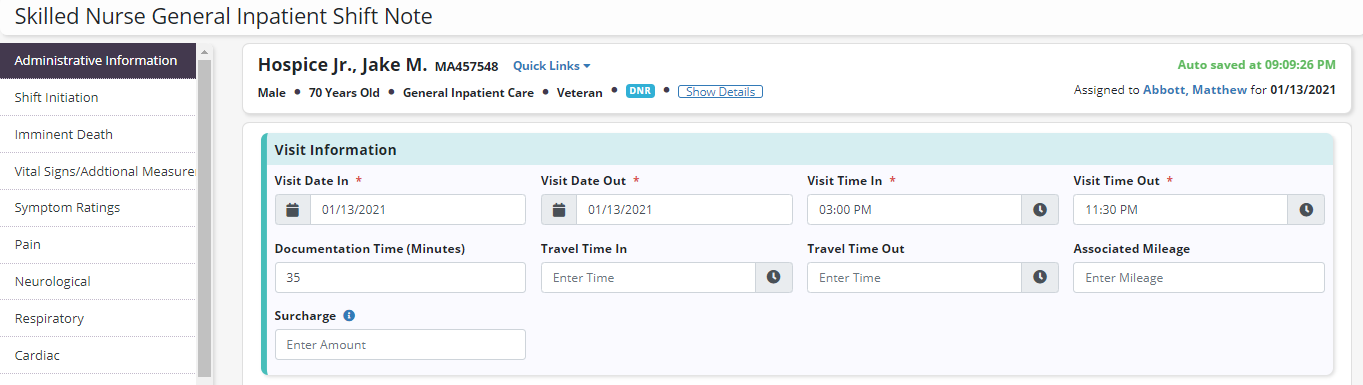
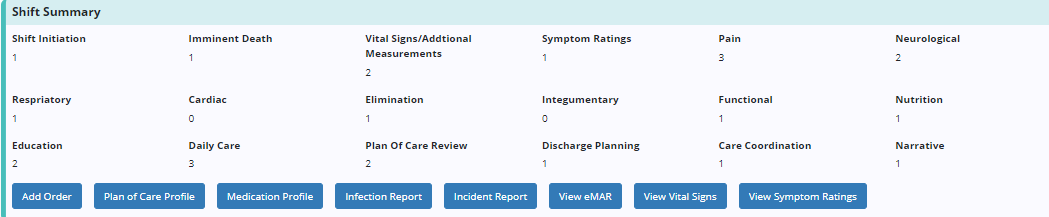
At the top of each tab, a Shift Summary section displays the total number of assessments completed during the shift.
Below the assessment tracking are action buttons that give users easy access to perform actions throughout the shift.
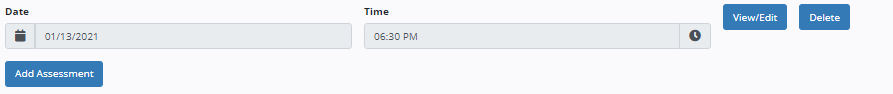
Users can complete multiple assessments throughout a shift. To add an assessment, click Add Assessment. The date and time of the assessment will appear in the Date and Time fields. To edit the date, time or assessment details, click View/Edit. Click Delete to delete an assessment.
In addition to the assessment information found in other skilled nursing documentation, users can complete documentation that is unique to shift work in these notes, including shift initiation, education, daily care and discharge planning.
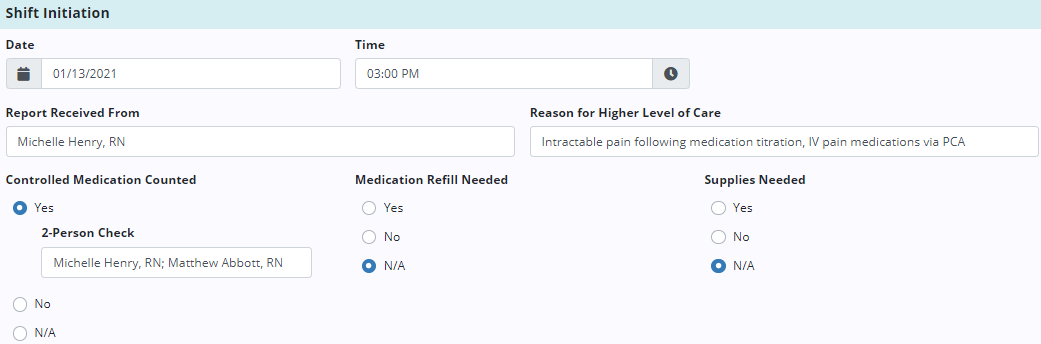
The Shift Initiation tab enables users to document tasks completed at the beginning of the shift as well as vital information, such as the reason the patient is receiving general inpatient or continuous care.
The Education tab enables users to document education provided by the nurse throughout the shift.
To document an education assessment, click Add Assessment. Click View/Edit to edit the date/time and enter details of the teaching performed, including knowledge deficits and medication teaching completed.
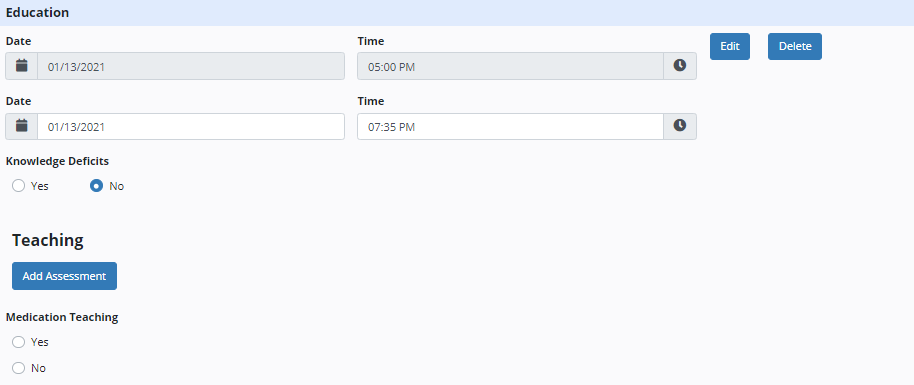
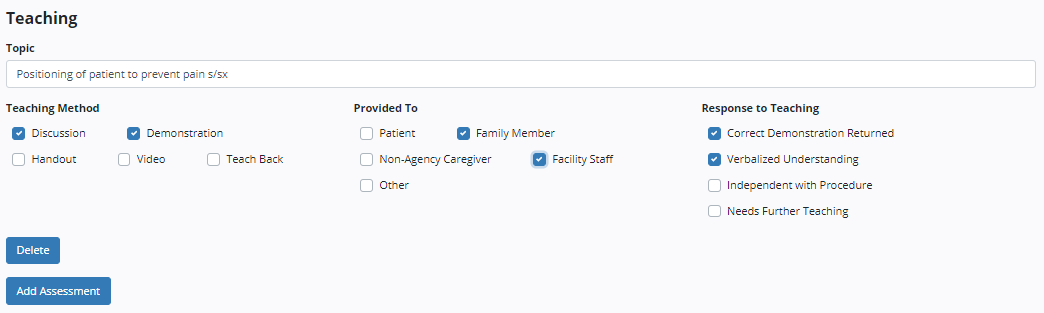
Under Teaching, click Add Assessment to add a teaching topic covered during the shift. Enter the topic, teaching method, response to teaching and the person who received the teaching. To add another topic, select Add Assessment. To remove a topic, click Delete.
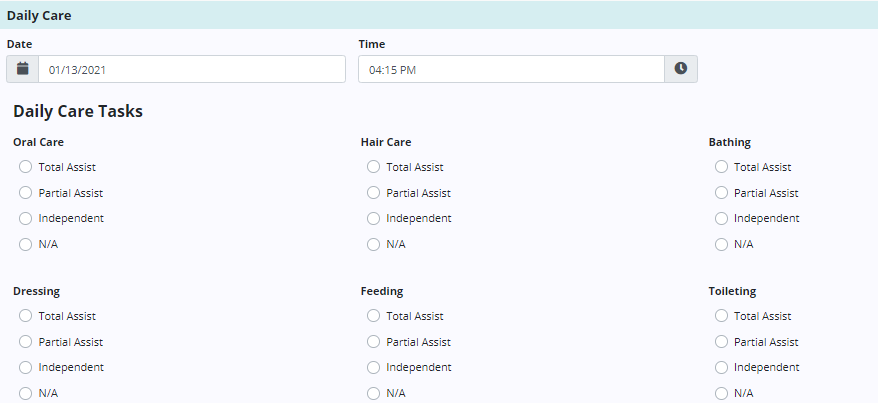
The Daily Care tab enables users to document personal care tasks performed during the shift. When documenting each task performed, users can select the level of assistance required by the patient.
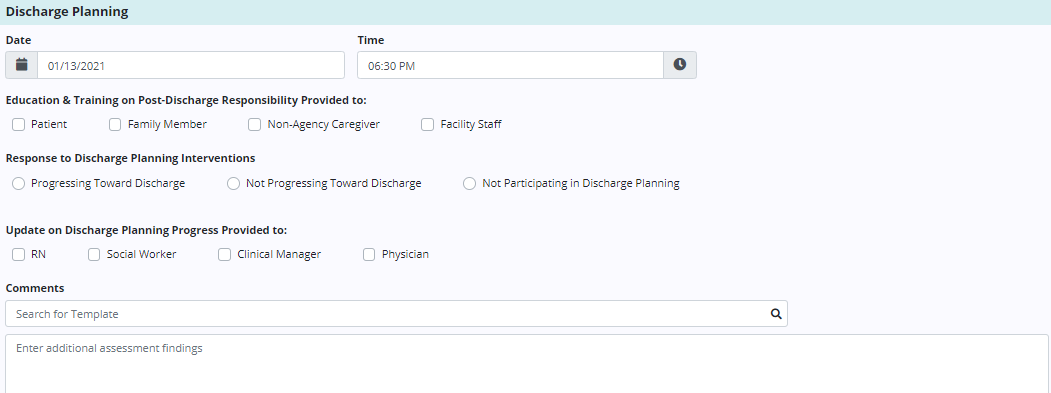
The Discharge Planning tab enables users to document information about discharge planning for patients receiving general inpatient or continuous care. Discharge planning documentation is critical to staying compliant.
Updated on 01/20/2021