The Quality Assurance (QA) Center is where clinical documentation is processed. When a clinician completes documentation, the documentation will appear as tasks in the QA Center for QA staff to review. QA staff can review, approve, and return documents in the QA Center. Agencies may choose to designate a Clinical Manager, Director of Nursing, or other supervisory personnel to handle QA review.
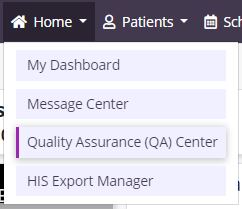
Select Quality Assurance (QA) Center under the Home tab to enter the QA Center.
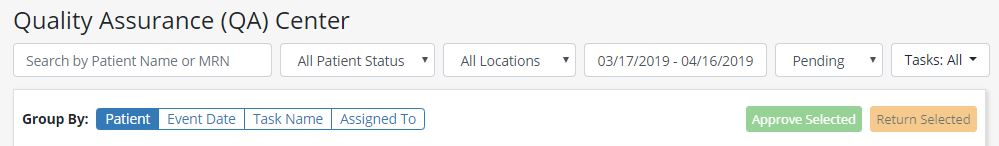
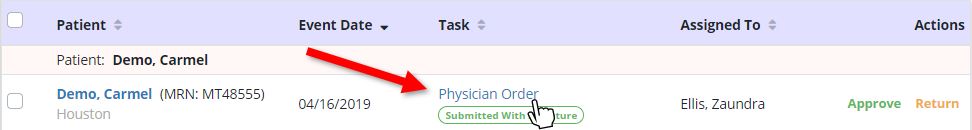
The default view when entering the QA Center shows active patient tasks that are ready for processing with an event date within the last month. QA staff can use the filters at the top of the screen to filter by Patient, Status, Branch, Date, Task Status, and Task. Each column can also be arranged in ascending or descending order.
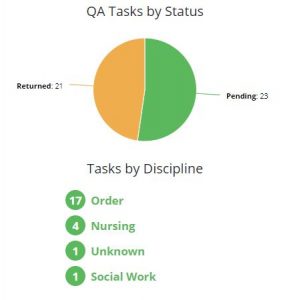
The tile on the right side of the screen displays a pie graph of Pending and Returned tasks. Users can select a section of the pie to view tasks in that status. When the user selects the orange Returned section, the screen will show only the list of returned documents.
Select a task name to preview a task for quality assurance.
A preview version will appear for review. At the bottom of the task window, users can select Approve, Return, or Back to QA Center.

NOTE: When reviewing an RN Initial/Comprehensive Assessment or RN Comprehensive Assessment, the QA reviewer will have additional items to review for the HIS Admission document. When reviewing a Discharge Visit, Unattended Discharge Note, Death Visit, or Unattended Death Note, there will be an additional HIS Discharge Document for review.
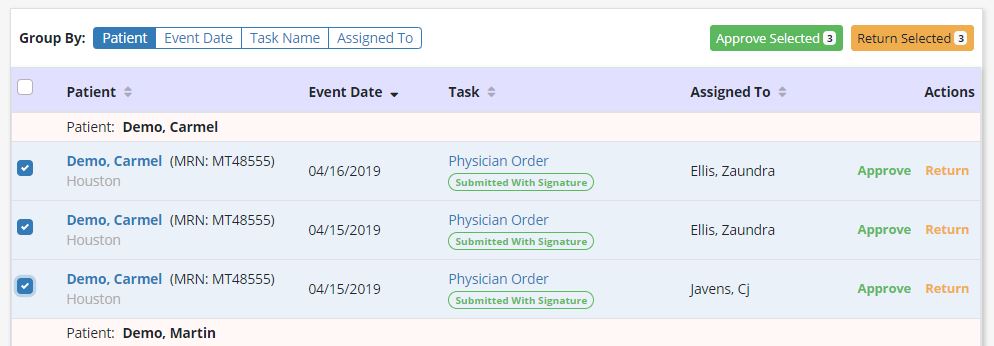
To approve or return multiple tasks, the QA review can also multi-select using the checkboxes on the left side of the screen. Once selected, the option to approve or return are available, along with the number of tasks selected.