Axxess Hospice now provides a Plan of Care Documentation button in all visit notes. When clicked, this button enables users to populate the Interventions Performed This Visit and Progress Toward Goals sections in the visit note with information from the plan of care.
This enhancement streamlines operations and facilitates thorough, accurate documentation.
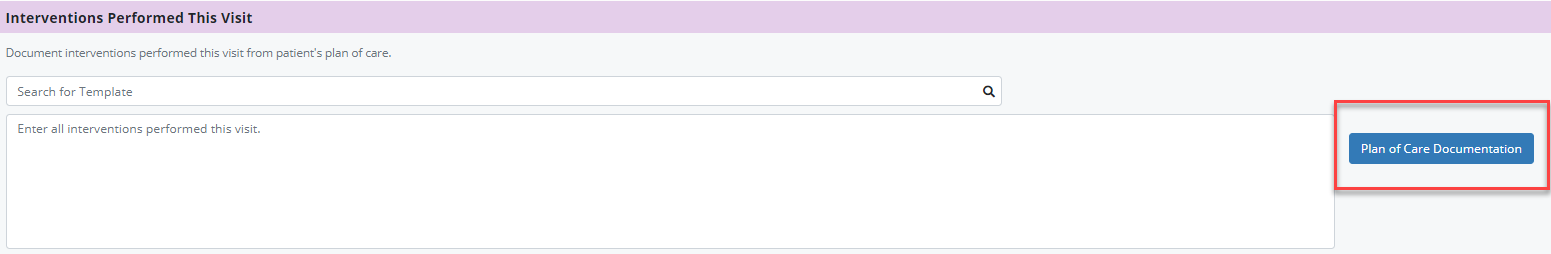
To document goals and interventions from the plan of care within a visit, open the visit, navigate to the Interventions Performed This Visit section and select Plan of Care Documentation.
Visit ➜ Interventions Performed This Visit section ➜ Plan of Care Documentation
Once Plan of Care Documentation is selected, a drop-down will appear above Interventions Performed This Visit. The drop-down will display each problem statement on the plan of care with its respective goals and interventions.
Select Document next to the goal or intervention you wish to document. Once Document is selected, the respective problem statement will flow to the Interventions Performed This Visit and Progress Toward Goals sections of the visit note. Users will only see problem statements with effective dates that are prior to or on the effective date of the visit.
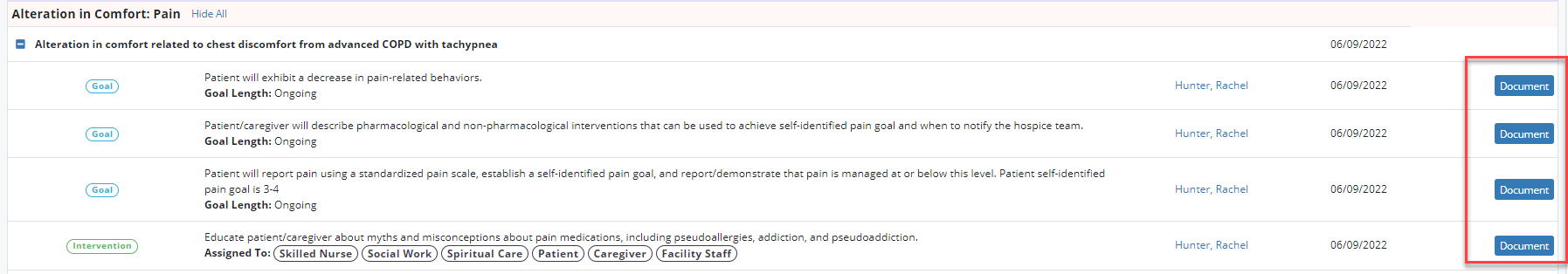
Once all the appropriate interventions and goals have been documented, select the Plan of Care Documentation button again to hide the plan of care problem statements.
To document goals and interventions from the plan of care within a Skilled Nurse Continuous Care Shift Note or Skilled Nurse General Inpatient Shift Note, navigate to the Plan of Care Review tab. In the Interventions Performed This Visit section, select Plan of Care Documentation.
Skilled Nurse Continuous Care Shift Note/Skilled Nurse General Inpatient Shift Note ➜ Plan of Care Review tab ➜ Interventions Performed This Visit section ➜ Plan of Care Documentation
Updated on 03/09/2023