The recommended visit type is the RN Comprehensive (HUV) HOPE Assessment; however, any visit documented within the HUV 1 or HUV 2 time frames can be used. It’s important to note that the RN Comprehensive (HUV) HOPE Assessment form includes a built-in scrubber, which can help ensure data accuracy and completeness. Using this form during the HUV periods may offer operational advantages, but the decision ultimately depends on your organization’s internal procedures and preferences.
Yes. If the RN Initial Assessment – HOPE is used to admit a patient, the RN Comprehensive Admission Assessment – HOPE must also be completed.
Begin by documenting the RN Initial Assessment – HOPE.
The RN Comprehensive Admission Assessment – HOPE can only be scheduled once during the admission period.
If the RN Initial Assessment – HOPE has already been scheduled, the RN Comprehensive Admission Assessment – HOPE must be completed within five days of admission.
Any visit type can be used to document a Symptom Follow-up Visit except for telehealth nursing visits.
When a patient requires a same-day SFV and dies on that same day, the system may not automatically recognize the scheduled Skilled Nursing Visit as valid for SFV documentation. This is because the system relies on visit time stamps to determine whether the SFV occurred after the initial symptom impact assessment. To ensure proper documentation:
Open the Skilled Nursing Visit in the system.
Enter a start time that is after the time of the symptom impact assessment.
Save and close the visit.
Document the missed visit with the appropriate SFV reasons.
Simply scheduling the visit and marking it as missed will not work unless the system can confirm that the visit was intended to occur after the symptom impact assessment. This manual time entry ensures the system categorizes the visit correctly and allows for accurate SFV documentation.
Access to the HOPE Center requires specific user permissions. Navigate to the People Center under the People tab to ensure your profile includes the appropriate permissions.
HOPE guidelines don’t require additional Symptom Follow-up Visits; however, organizations should follow their internal policies and procedures to schedule a follow-up visit.
The system retains the first recorded answer to a question. If a later visit provides a different response, users have the option to replace the original answer with the updated one.
If the new answer is the same, no replacement occurs.
If validation errors or warnings are present, reviewers can replace the answer to resolve those issues.
Prerequisite: All visits associated with the record must be closed.
Navigate to the HOPE Export Manager ➜ Export Ready tab
Click Export to generate the HOPE export file.
Review the XML data.
Submit the record to iQIES.
Mark the record as Exported.
Update the status to Accepted or Rejected based on the iQIES validation report.
Before marking the record as Accepted or Rejected on the Export History screen, users have one final chance to generate the file via the three-dot menu option.
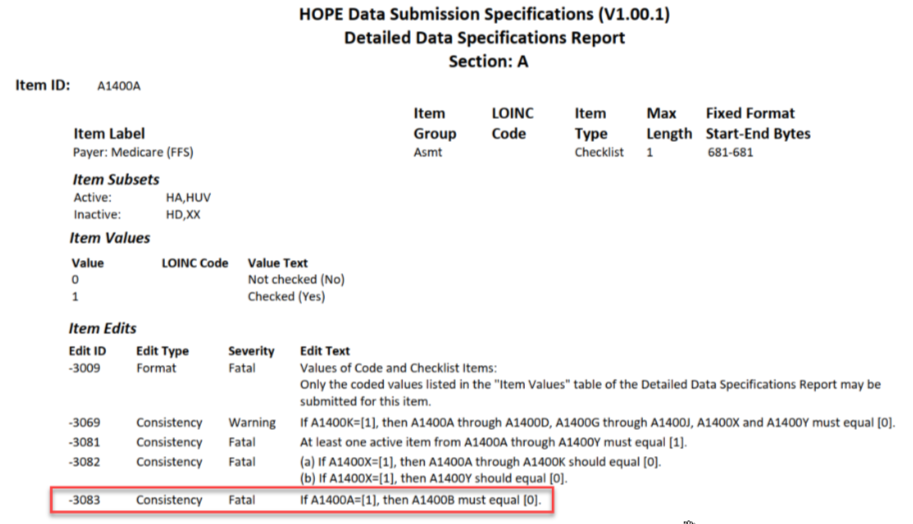
This issue relates to item A1400 in the HOPE Data Submission Specifications V1.001. According to these specifications, users cannot select both Medicare (A1400A) and Medicare Advantage/Part C (A1400B). This is a change from the previous HIS specifications.
While the HOPE manual suggests selecting both options if the patient had Medicare Part C before enrolling in hospice, doing so currently triggers a fatal error in the Validation Utility Tool (VUT). The scrubber logic follows CMS’ official specifications. Until CMS provides further clarification, users must choose either traditional Medicare or Medicare Advantage, not both.
Modification Request: Used to correct non-key fields.
Inactivation Request: Required for changes to key demographic fields such as:
First and Last Name
Date of Birth
Social Security Number
Event Date
No. The Z0500B date must remain unchanged even after modifications are made.