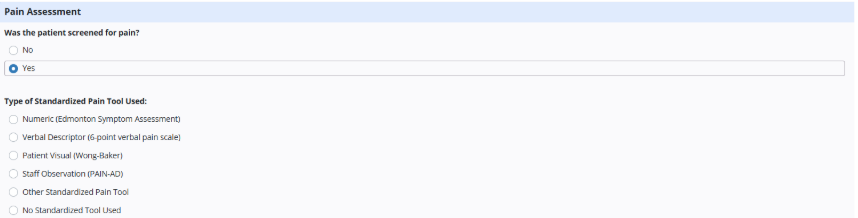
Axxess Hospice now provides a pain and symptom management module with rating assessments for visits.
The following nursing assessments use the following standardized tools: Numeric (Edmonton Symptom Assessment), Visual Descriptor (6-point verbal pain scale), Patient Visual (Wong-Baker), Staff Observation (PAIN-AD), Other Standardized Tool Used and No Standard Tool Used.
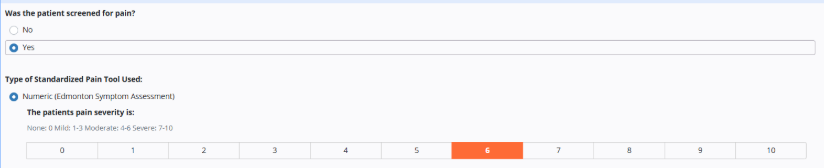
Numeric (Edmonton Symptom Assessment)
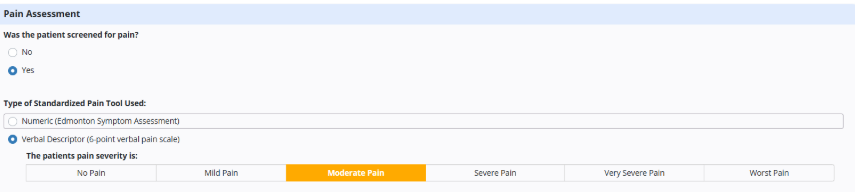
Verbal Descriptor (6-point scale)
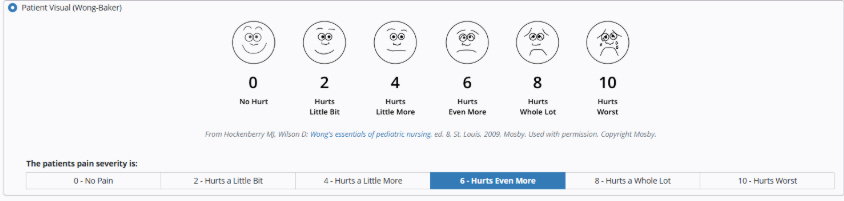
Patient Visual (Wong-Baker)
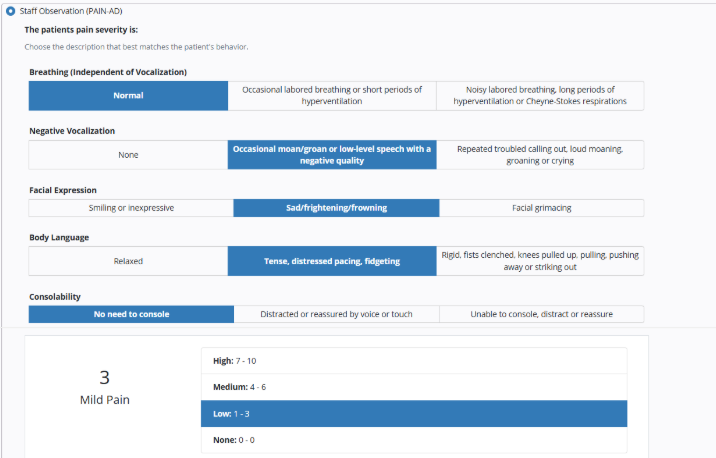
Staff Observation (PAIN-AD)
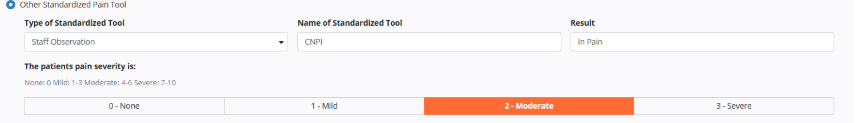
Select Other Standardized Pain Tool if a different pain tool was used. Select the type of tool, enter the name and result and select the pain severity.
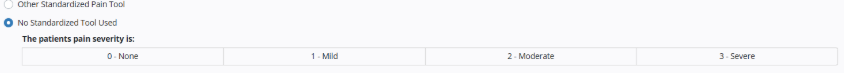
Select No Standardized Tool Used if a tool wasn’t used and select the pain severity.
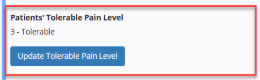
To update a patient’s pain level, navigate to the Clinical Information tab in the patient’s chart, select the pain level in the Tolerable Pain Level section and click Save.
Patients tab ➜ Patient Chart ➜ Edit Profile ➜ Clinical Information tab ➜ Tolerable Pain Level ➜ Save
Users can also select Update Tolerable Pain Level.
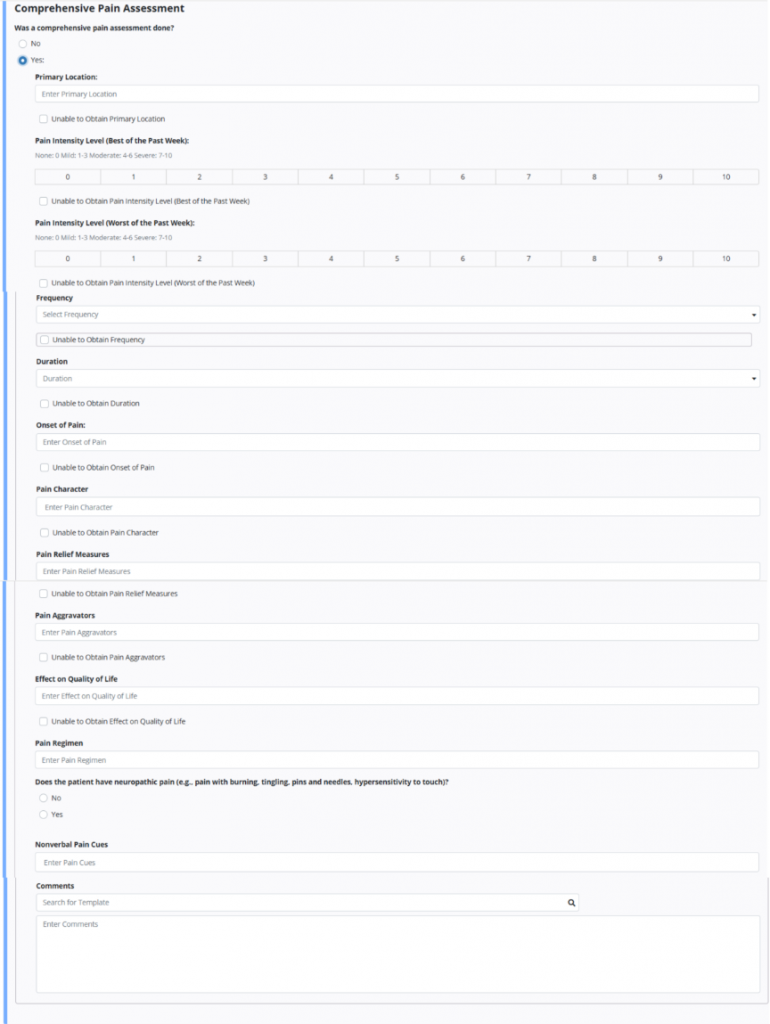
If a comprehensive pain assessment was completed, select Yes. This section is required at admission for HOPE documentation.
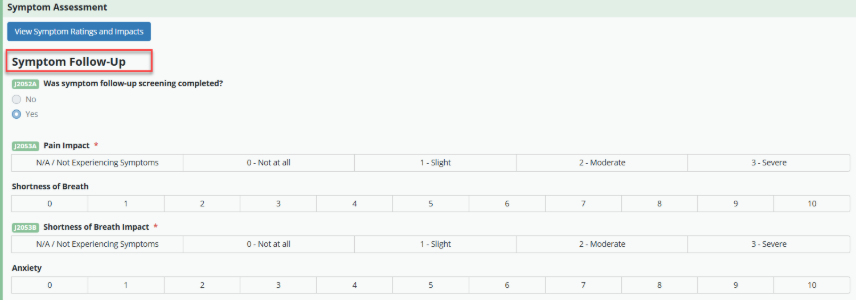
The Symptom Impact Assessment enables users to document the impacts of pain, anxiety, constipation, shortness of breath, nausea, vomiting, diarrhea, agitation, HUV between days 6-15 and HUV between days 16-30. A symptom follow-up visit is required if a a symptom impact is between 2-Moderate and/or 3-Severe.

If a follow-up visit is required, users will receive the following message:
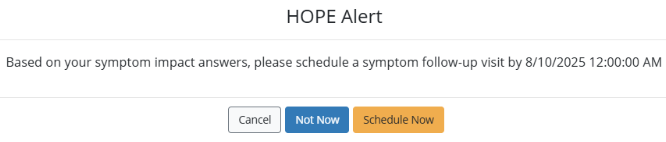
Any in-person nursing visit (RN, LVN, or LPN) can be used as a symptom follow-up visit. When the visit is opened, the module will automatically categorize it as a symptom follow-up assessment and require documentation by the clinician.