Axxess Home Health now provides no-pay RAP and 2021 billing settings for episodic payers, so organizations can easily identify payers that follow CMS 2021 RAP requirements. This functionality streamlines claims processing and facilitates compliance with the 2021 billing changes.
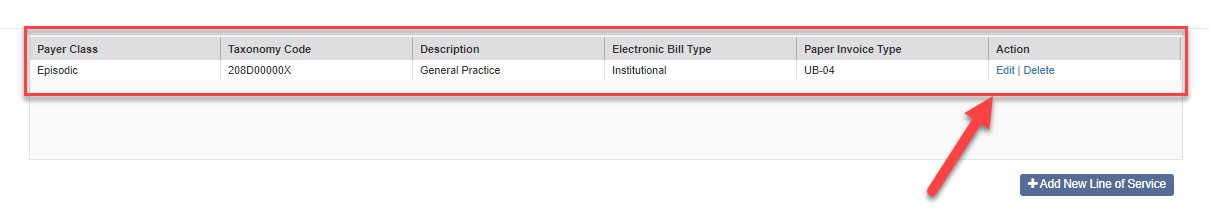
To enable the new episodic payer settings, edit the payer’s profile and navigate to the Payer Class table in the Insurance/Payer Details section. Click Edit in the Actions column to edit a line item.
View tab ➜ Lists ➜ Insurances/Payers ➜ Edit ➜ Payer Class table ➜ Edit
The following options now appear toward the bottom of the line item window:
Check this box to enable no-pay RAPs.
Check this box to follow CMS 2021 RAP requirements.
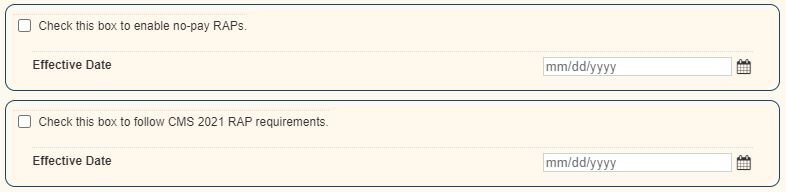
These settings cannot be enabled unless the above box is selected (Check here if the payer follows PDGM billing requirements.).
When enabling these settings, an effective date is required. The effective date cannot predate January 1, 2021. Additionally, when the no-pay RAP settings are enabled, claims with start dates on or after the effective date will be split at a 0/100% ratio for RAPs and finals.
Updated on 12/09/2020