Beginning 01/01/2022, Medicare will phase out RAPs and begin requiring a Notice of Admission (NOA) to be submitted once every admission period. A Notice of Admission must be submitted in the following scenarios:
|
New admissions |
|
|
Crossover patients |
Axxess has implemented a solution that can recognize both scenarios and automatically create the appropriate claims (RAP claim, final claim or Notice of Admission) for both instances.
Patients admitted to home health services in CY 2022 will require a Notice of Admission to be submitted within five days of the episode start date to be considered timely. For every day after the fifth day of the billing period that the NOA is not submitted, the organization will be penalized 1/30th of the final payment.
Organizations that do not submit a timely Notice of Admission will face a minimum 20% reduction in final payment. This will match the current penalty implemented in CY 2021 for RAPs. The Notice of Admission will only be required once per admission period. Once the Notice of Admission is accepted, all subsequent billing periods will only require a final claim to be submitted.
Patients who are admitted prior to 01/01/2022 and remain on service will require a one-time Notice of Admission to be created on the first billing period that starts on or after 01/01/2022.
Example: A patient is admitted or recertified and has an episode range of 12/25/2021-02/22/2022. The first 30-day billing period is 12/25/2021-01/23/2022 and would have a RAP and final claim created and needed for submission. The second 30-day billing period is 01/24/2022-02/22/2022. Because the billing period start date begins in CY 2022, the billing period will create a one-time NOA and a final claim needed for submission. If the patient is again recertified in February resulting in an episode of 02/23/2022-04/23/2022, each billing period will only create a final claim as the NOA for the admission was already submitted in the prior period.
Once the system generates a Notice of Admission, the submission process will be identical to the RAP submission process.
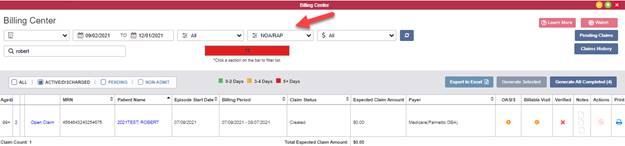
To submit a Notice of Admission, navigate to the Billing Center under the Billing tab. Select NOA/RAP from the drop-down menu at the top of the screen and click Open Claim next to the desired claim.
Billing tab ➜ Billing Center ➜ NOA/RAP ➜ Open Claim
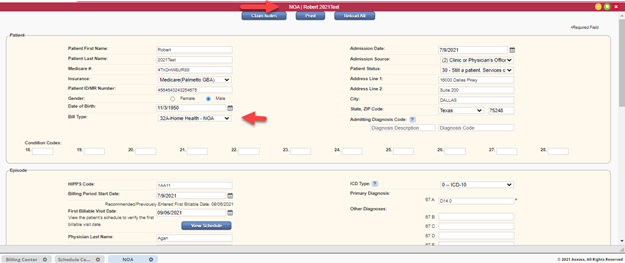
The claim will open with the bill type listed as 32A-NOA and the claim details automatically populated. Review the claim information to verify accuracy and click Verify.
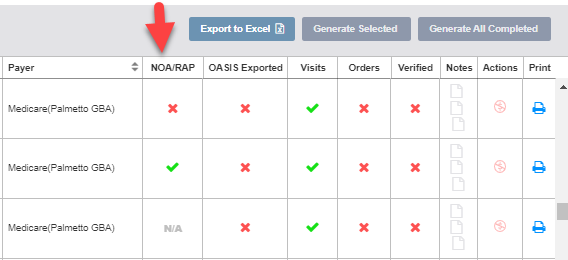
Once verified, submit the Notice of Admission by checking the box next to the claim and clicking Generate Selected.

When submitting a final claim, the RAP validation checks have been modified to include the Notice of Admission.
Billing periods prior to 2022 will check to verify that the RAP has been submitted before the biller can verify the final claim.
Billing periods on or after 01/01/2022 that have an NOA within the same billing period as the final will validate that the NOA has been submitted before enabling the biller to verify the final claim.
Billing periods on or after 01/01/2022 that do not have an NOA in the same billing period will not perform any checks against a RAP or NOA.
For Medicare HMO (episodic) payers, several toggles are available depending on the specific payer requirements.
Option 1: Payer continues to accept RAPs.
If the payer opts to continue accepting RAPs in CY 2022, no further action is required. The same payer setup used for claims in CY 2021 will continue to be allowed and Axxess will continue generating the RAPs and finals as defined in the payer profile.
Option 2: Payer requires the Notice of Admission.
If the payer opts to follow the CMS requirements for a Notice of Admission to be created and submitted on admission or on the first billing period for crossover patients, edit the payer to indicate that NOAs are required.
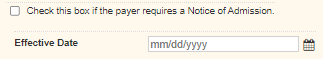
To indicate that NOAs are required for a payer, navigate to the Insurances/Payers list and edit the payer. Edit the line of service and check the box next to Check this box if the payer requires a Notice of Admission. Enter the effective date and click Save.
View tab ➜ Lists ➜ Insurances/Payers ➜ ![]() ➜ Edit line of service ➜ Check this box if the payer requires a Notice of Admission ➜ Effective Date ➜ Save
➜ Edit line of service ➜ Check this box if the payer requires a Notice of Admission ➜ Effective Date ➜ Save
The effective date will only accept dates on or after 01/01/2022.
Once enabled, the system will stop generating RAPs for newly created billing periods that start on or after the effective date entered. The system will generate NOAs for new admissions beginning on or after the effective date and a one-time NOA for active patients crossing over the effective date. Crossover patients (patients active prior to the effective date) will have a Notice of Admission created for the first billing period that begins on or after the effective date.
Note: If the toggle is enabled after episodes that fall within the effective date are already created, the NOA will NOT be automatically created. It is important to verify with your payers and enable the toggles as needed to avoid having to manually delete and create claims.
Option 3: Payer only requires final claims.
If the payer opts to discontinue RAPs, does not require a Notice of Admission, and only requires a final claim to be submitted every billing period, users can enable the appropriate setting by editing the payer’s line of business and checking the box next to Check this box if the payer does not require RAPs/Notice of Admission.
View tab ➜ Lists ➜ Insurances/Payers ➜ ![]() ➜ Edit line of service ➜ Check this box if the payer does not require RAPs/Notice of Admission ➜ Effective Date ➜ Save
➜ Edit line of service ➜ Check this box if the payer does not require RAPs/Notice of Admission ➜ Effective Date ➜ Save
All billing periods created before the effective date will have a RAP and final created automatically and all billing periods created on or after the effective date will only have a final claim created.
Updated on 12/09/2021