System-wide workflow automation features have been integrated throughout the Home Health solution to streamline agencies’ operations during and after the transition to PDGM.
Screenshots and content for pending features will be added progressively. Continue to check this page and other subsections of our PDGM content using the left-side menu. Axxess will continue to notify you as PDGM feature developments occur and new features become ready for use.
Billing automation enables clients to submit claims faster and maintain efficient, optimal cash flow to fulfill 30-day billing requirements under PDGM, without having to onboard additional billers.
Visit the PDGM Billing Center section for additional information on billing automation for PDGM.
Real-time validations compare physical assessment findings to OASIS items and automatically disable non-applicable items to prevent clinicians from entering contradictory documentation. This functionality enables users to complete documentation faster and more accurately and spend less time on QA review.
Enable Real-Time Validations
Once enabled, validations will happen in real-time as clinicians complete documentation. Validations occur at all OASIS time points and for all disciplines.
For example, if a clinician documents Dyspnea in a patient’s Respiratory Assessment, the non-applicable options on M1400 will be disabled. Non-applicable items include:
Non-applicable items are grayed out and cannot be selected, as shown in the following screenshot:
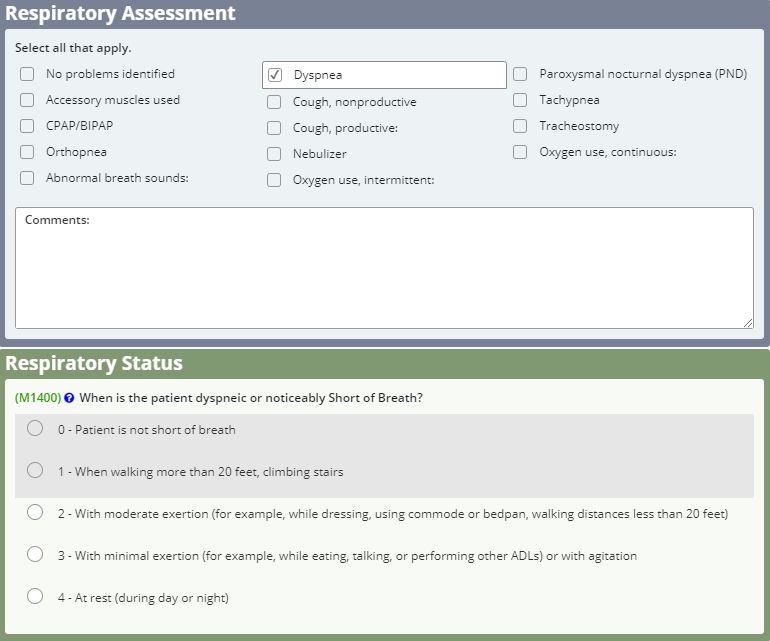
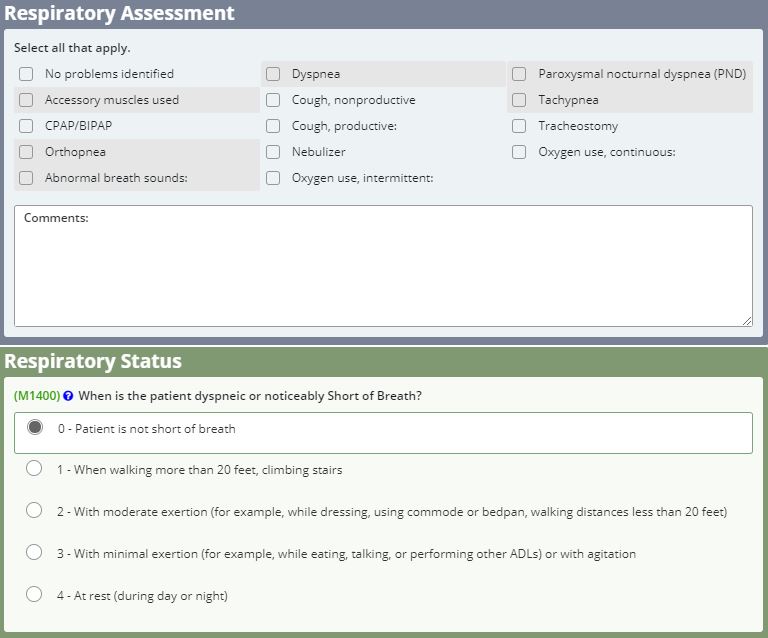
If the clinician indicates in the OASIS assessment that a patient is not short of breath, non-applicable items are grayed out in the Respiratory Assessment. Non-applicable items include:
When a clinician documents Neuro/Behavioral Status, non-applicable OASIS options on M1700 and M1710 are disabled until the patient’s orientation is documented.
As soon as orientation is documented, these OASIS responses are enabled.
Real-Time Validations Functionality
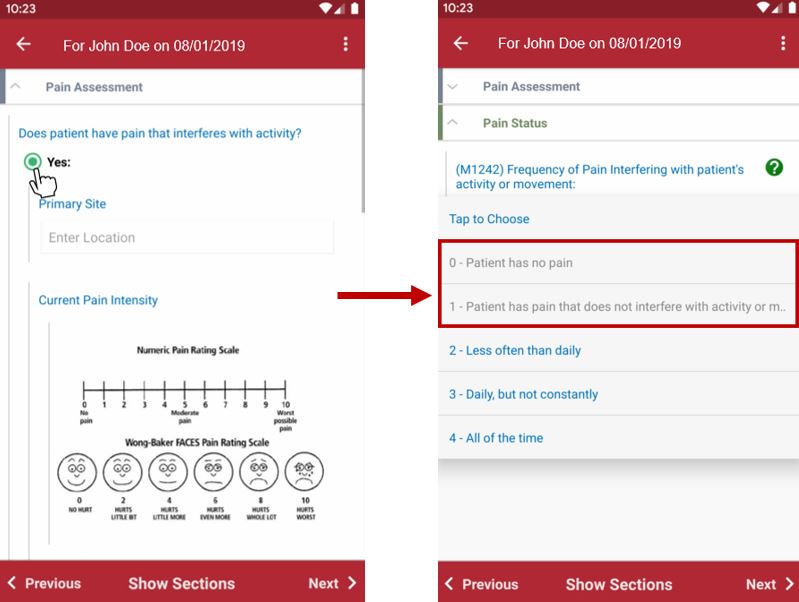
Mobile Validations
The example below shows real-time validations on a mobile application. When the user indicates that the patient has pain in the Pain Assessment, non-applicable items on M1242 are grayed out in the OASIS. Non-applicable items include:
Using the Change in Focus form, agencies can easily document when a patient’s primary diagnosis is resolved and another existing diagnosis becomes the focus of care.
The Change in Focus form must be used within the first 30 days of the episode to update the focus of care for the second 30-day billing period. Change in Focus forms and OASIS assessments have equivalent weight as they relate to claims. When completed after the most recent OASIS, the Change in Focus form provides diagnoses for the appropriate claims.
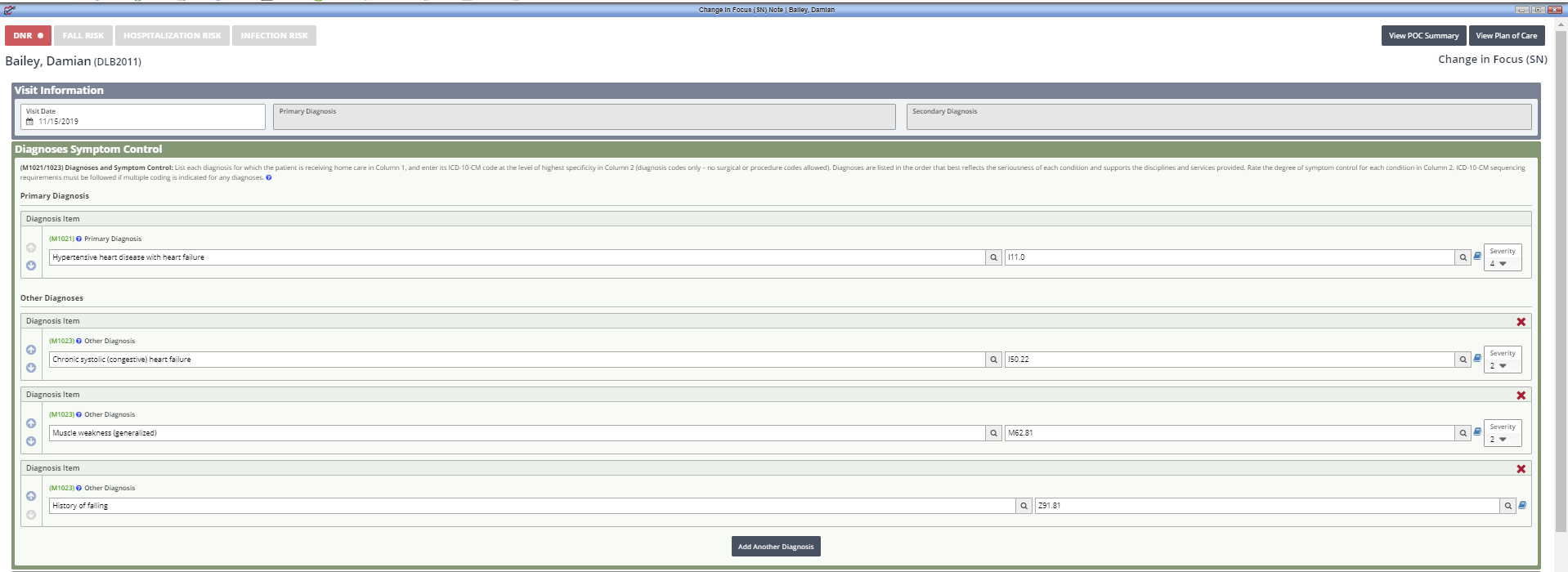
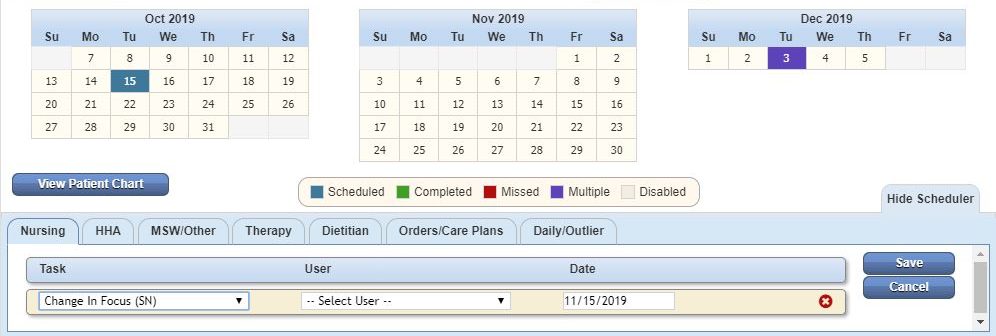
Create a Change in Focus Form
To document a patient’s change in focus, create a Change in Focus form in the Schedule Center. Navigate to the Schedule Center under the Schedule tab and select the appropriate Change in Focus task from the Task drop-down menu.
Schedule tab ➜ Schedule Center ➜ Select Visit Type in Task menu ➜ Change in Focus
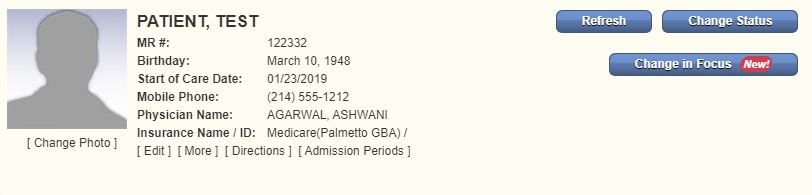
Change in Focus in Patient Charts
Users also have convenient access to Change in Focus forms through the Patient Charts.
Patients tab ➜ Patient Charts ➜ Change in Focus button
Calculate Case-Mix
On the Change in Focus form, the Calculate Case-Mix button is available to users who have permission to see financial data. When selected, the PDGM Case-Mix Analysis opens to display the new case-mix calculation based on the patient’s updated diagnosis sequencing and most recent OASIS data for admission source and timing and functional impairment.
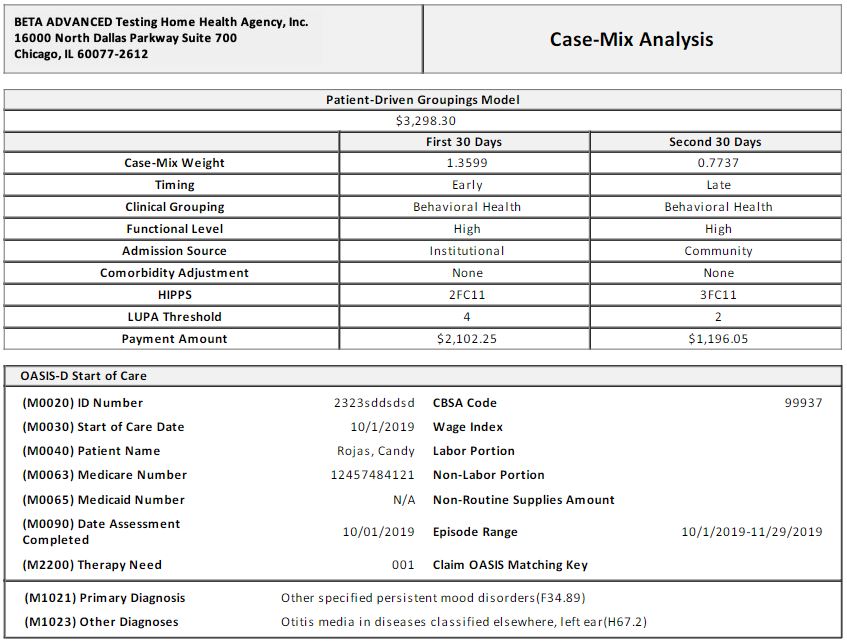
Case-Mix Permissions:
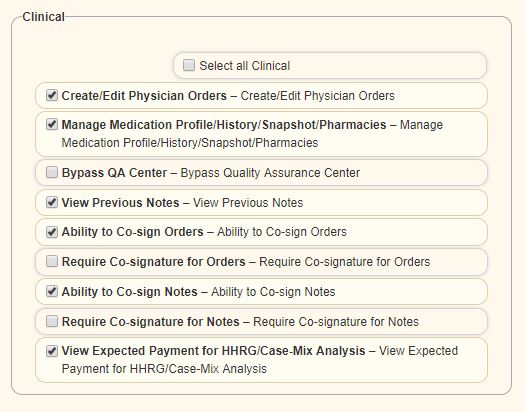
To give a user permission to access case-mix data, navigate to the Permissions tab in the user’s profile. In the Clinical permissions section, select View Expected Payment for HHRG/Case-Mix Analysis. Once this permission is granted, the user will be able to see the Calculate Case-Mix button to generate case-mix data in the Change in Focus form.
View tab ➜ Lists ➜ Users ➜ Edit ➜ Permissions tab ➜ Clinical section ➜ View Expected Payment for HHRG/Case-Mix Analysis
Significant changes in a patient’s condition should be documented using an OASIS Follow-Up assessment.
The Wound Manager enables users to manage multiple wounds from a central location. In addition to managing supplies, wound orders, wound documentation and disposable NWPT devices, users can access valuable insights into the quality and financial impact of wound care through the Wound Manager.
During the intake process, alerts notify you instantly if a diagnosis is payable under PDGM, so you know immediately if more information is required to generate a payable code. This system enhancement enables you to decide at intake if a patient is eligible for home health services, and protects your revenue for the care your agency provides.
An overview of updates made to the intake forms in preparation for PDGM is provided below:
Demographics Tab
Admission Source and Timing have been added to the intake process in preparation for PDGM. It is vital that this information is entered into the system correctly. This information will be the basis of several reports and PDGM projection tools at intake.
The information entered here will flow to the OASIS assessment.
Clinical/Diagnoses Tab
Primary Diagnosis is now required in Axxess’ Home Health solution.
Referral Tab
Selecting a face-to-face encounter option is now required in the Home Health solution. For insurance types that require a face-to-face encounter visit (e.g., Medicare, Medicaid), the date of the physician encounter is required as a part of the certification statement on the Plan of Care. Two responses are available:
A third response option (N/A) is available when face-to-face documentation is not required by the insurance payer.
Tool tips provide additional information and resources for understanding face-to-face regulations.
Click the video below to watch an overview of the Intake Form Updates:
Orders-driven scheduling enables agencies to optimize operations in the following ways:
Set Up Orders-Driven Scheduling
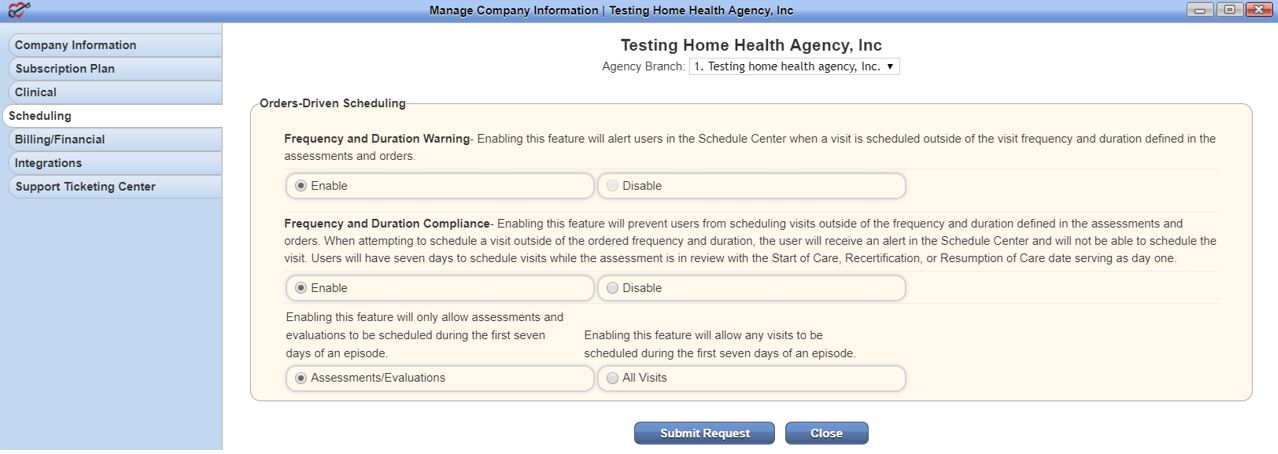
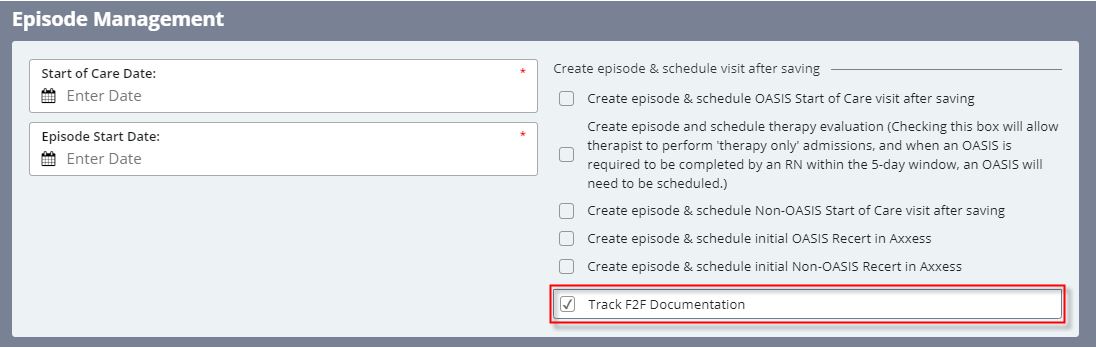
Functionality
Once the features are enabled, all visits will require an order before scheduling. Any new episodes will have calendars that are greyed out, except the first seven days of the episode.
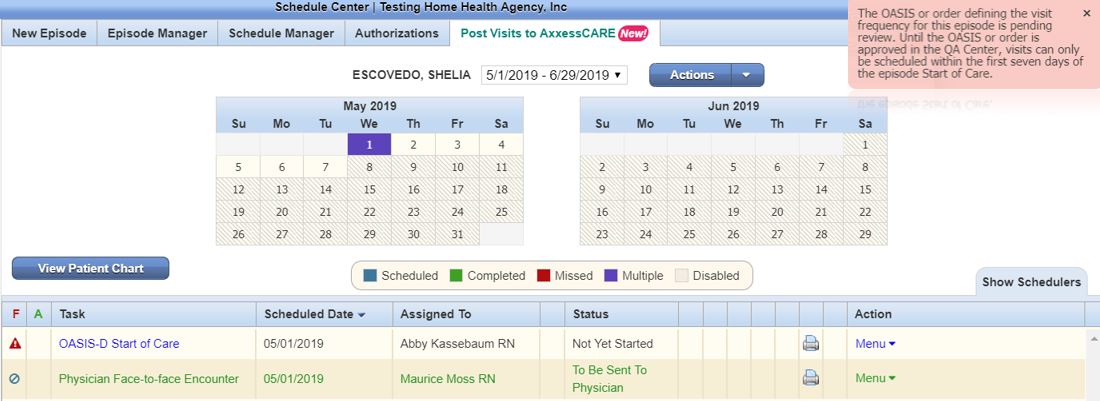
Visits scheduled and performed in the first seven days of the episode will have a frequency warning symbol in the Schedule Center, until the OASIS is approved.
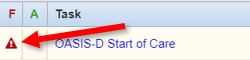
Once approved, the warning will be replaced with a green check mark symbol (as long as the visit falls within the ordered frequency).
Once all visits are scheduled, users can access the Frequency and Duration Summary in the Schedule Center, to quickly determine whether a visit was scheduled according to the ordered frequency.
Schedule Center ➜ Episode Manager ➜ Frequency and Duration Summary
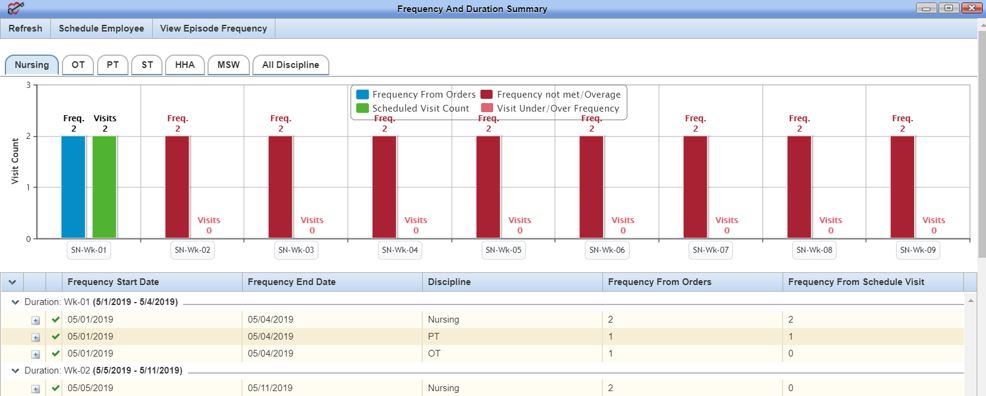
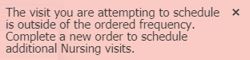
If the user attempts to schedule more than the ordered number of visits for a given frequency, a warning message will instruct the user to complete a new order before scheduling further visits.
A new section of reports in the Report Center will provide PDGM-specific reporting.
Our integrations with WorldView and Doctor Alliance enable Axxess users to seamlessly and efficiently manage orders and documents for optimal productivity under PDGM.
Our integration with WorldView enables agencies to:
For additional information on WorldView, visit the WorldView Document Management section of the Help Center.
Our integration with Doctor Alliance enables agencies to: