The Billing Center enables users to manage all billing processes in a central location and streamline operations to ensure timely claim submissions.
Access the Billing Center
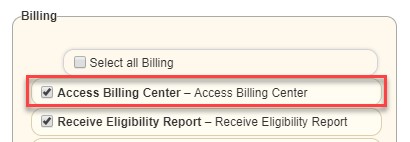
To access the Billing Center, users must have the Access Billing Center permission enabled.
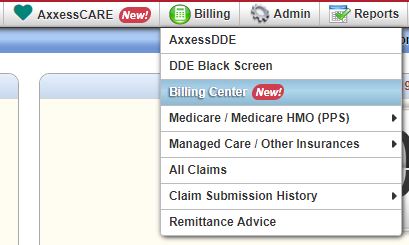
Users with this permission can navigate to the Billing Center under the Billing tab.
Benefits of the Billing Center
Billing Center Functionality
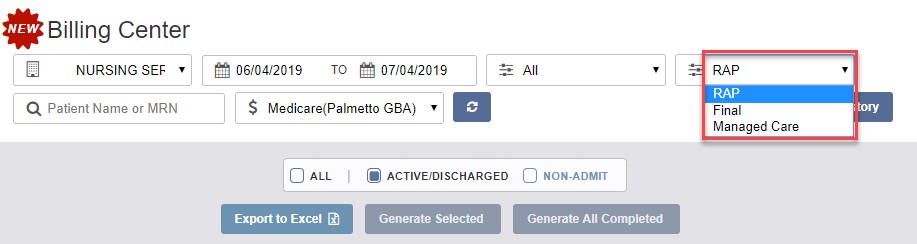
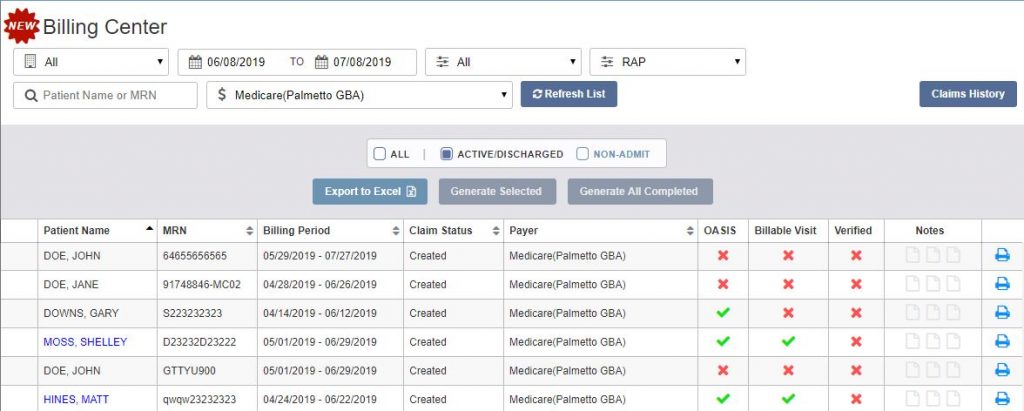
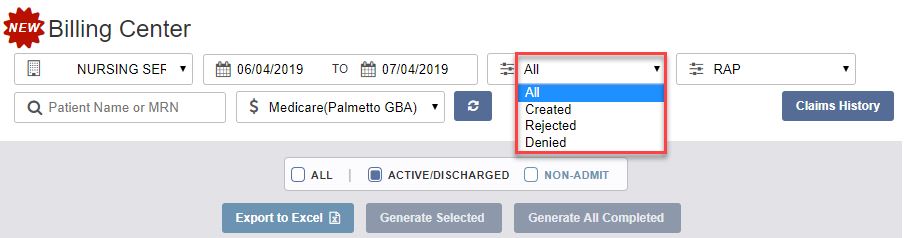
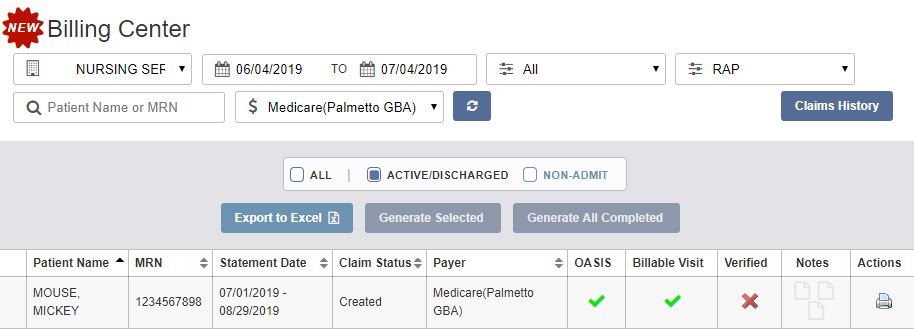
The Billing Center displays claims in Created, Rejected, and Denied status.
The same functionalities available in the previous Billing menu are available in the Billing Center.
A comorbidity adjustment is one of four primary components that comprise the PDGM regulations effective January 2020. When an agency assesses a patient under PDGM, all diagnoses will be taken into consideration to determine whether the patient is eligible for a low or high comorbidity adjustment, if any.
When a Medicare or Medicare HMO claim is selected for any patient, only the primary diagnosis is required, but users can also enter up to 24 additional diagnoses in the first step of the claim creation process.
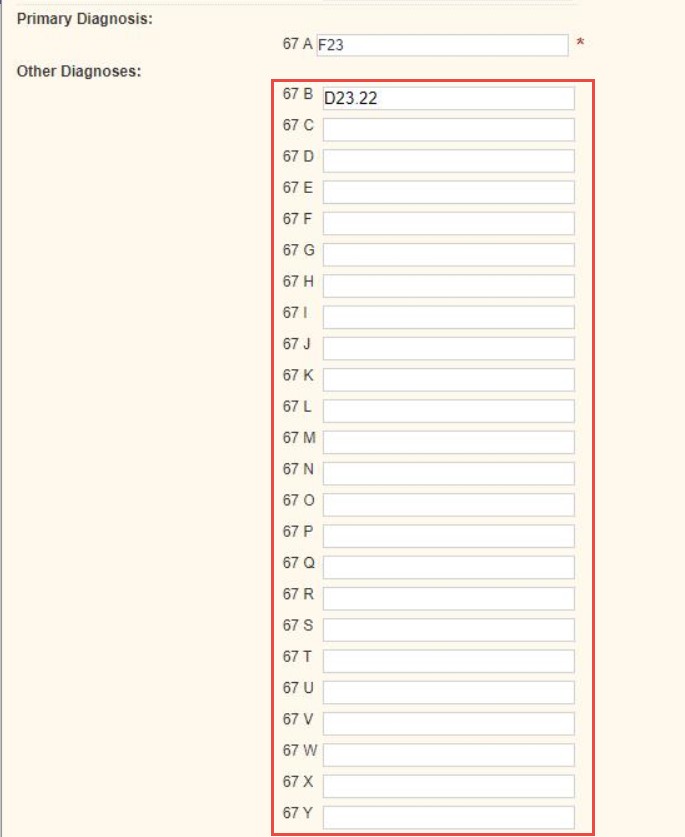
With the ability to provide all diagnoses that apply to a patient’s episode of care, agencies are better equipped to:
Additional information on PDGM can be found in the PDGM section of the Help Center and in the Axxess PDGM Resource Center.
Accounts receivable management is critical to financial health under PDGM. The Home Health solution enables users to assign a status to each RAP and Final claim (e.g., Paid, Submitted). In addition to the existing claim statuses, users can assign a Write-Off status to Medicare and Medicare HMO claims.
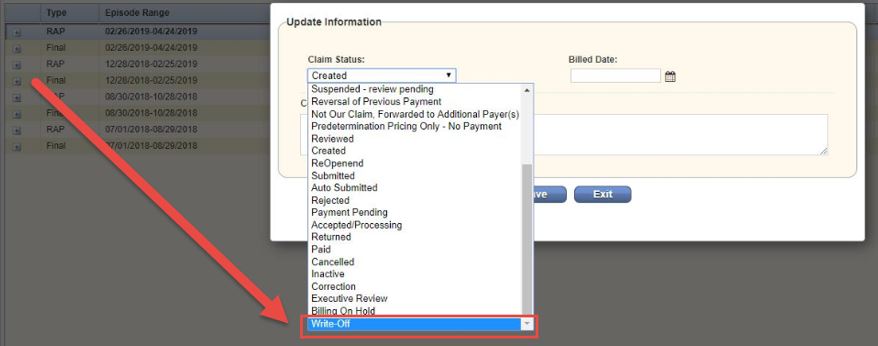
Claim statuses appear in A/R Roll Forward Reports, so users can communicate actions taken or actions needed on individual claim amounts.
Updated on 7/09/2019