PDGM Modeling Tool
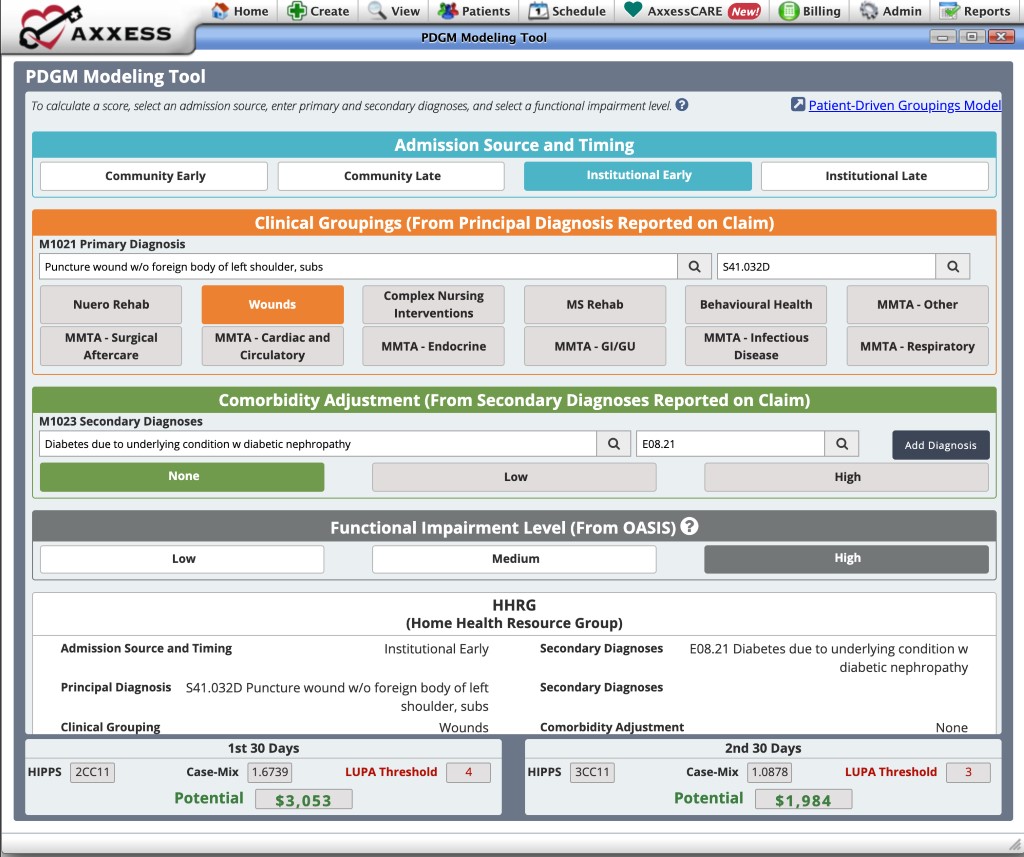
This interactive training tool is designed to help you learn how different factors generate the payment resource groupers under PDGM.
The tool is not tied to any patient, so each variable that impacts payment can be adjusted to give you targeted insights into how you can collect maximum reimbursement under PDGM.
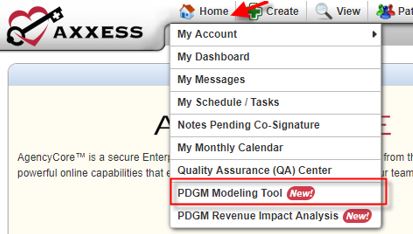
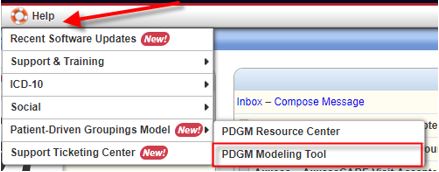
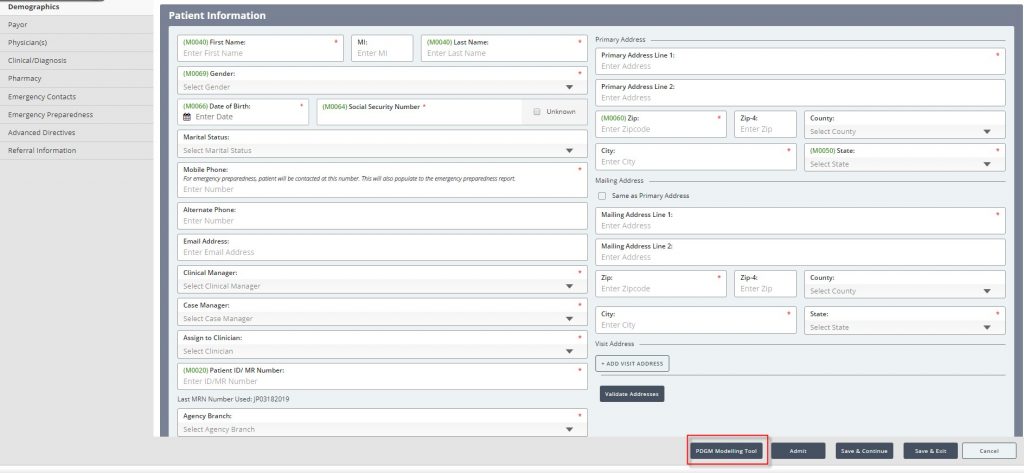
Accessing the PDGM Modeling Tool: All users have access to the modeling tool under the Home or Help tab, and when editing or creating a patient in Axxess AgencyCore.
From the Home tab:
From the Help tab:
From editing/creating a patient:
Admission Source and Timing
Payment periods are grouped by admission source (community versus institutional) and period timing (early versus late). Select one of the following to indicate the admission source and the timing of the admission:

Admission Source
Institutional:
- Acute (inpatient acute care hospitals), or
- Post-acute (skilled nursing facility, inpatient rehabilitation facility, long term care hospital, or inpatient psychiatric facility) care in the 14 days prior to home health admission
Community:
- No acute or post-acute care in the 14 days prior to home health admission
- 30-day periods with an institutional admission source were found to have higher resource use than periods with a community admission source.
Timing
Sequence of home health periods: Periods with no more than 60 days between the end of one period and the start of the next period (no change from current definition).
- Early periods: First 30-day period in a sequence of home health periods
- Late periods: Second 30-day period and later in a sequence of home health periods
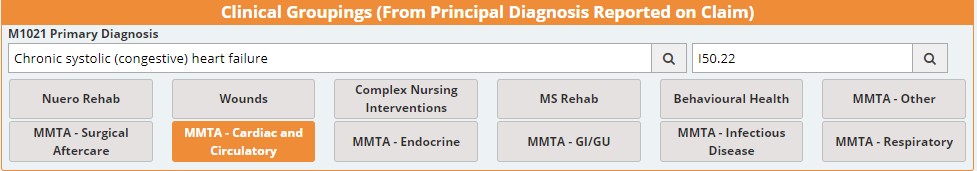
Clinical Groupings (From Principal Diagnosis Reported on Claim)
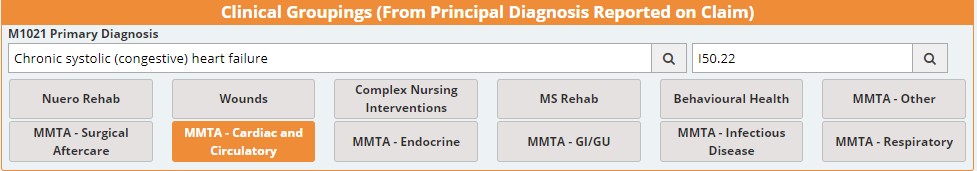
Clinical groups are intended to reflect the primary reason for home health services
- Defined by the principal diagnosis reported on home health claim
- Twelve total groups used in the PDGM
If a diagnosis code is used that does not fall into a clinical group (e.g., R-symptom codes or unspecified codes), the claim is not payable and returned to the provider for more definitive coding. Axxess warns agencies to not enter unpayable codes through out the software (starting at patient intake).
Enter a primary diagnosis. If the diagnosis is groupable, then a clinical grouping will be highlighted. If a questionable encounter code is entered, then a message will appear stating the code is not groupable.
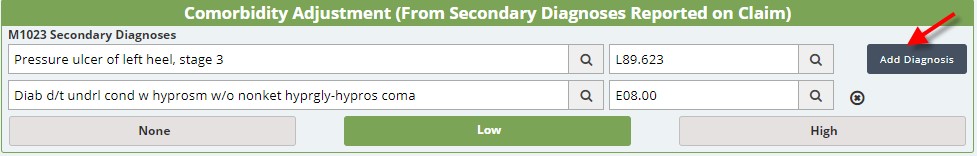
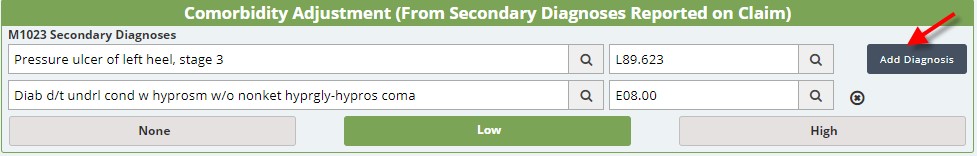
Comorbidity Adjustment (From Secondary Diagnoses Reported on Claim)
A comorbidity is defined as a medical condition coexisting in addition to a principal diagnosis. Comorbidity is tied to poorer health outcomes, more complex medical need and management, and higher care costs.
PDGM includes a comorbidity adjustment category based on the presence of secondary diagnoses.
A 30-day period may receive:
- Low comorbidity adjustment: There is a reported secondary diagnosis that is associated with higher resource use.
- High comorbidity adjustment: There are two or more secondary diagnoses that are associated with higher resource use when both are reported together compared to if they were reported separately. (The two diagnoses may interact with one another, resulting in higher resource use.)
- No comorbidity adjustment: There is no reported secondary diagnosis that falls in either the low or high comorbidity adjustment.
To obtain the comorbidity adjustment, enter secondary diagnoses. When a secondary diagnosis that represents a comorbidity adjustment is entered, then a low or high indicator will appear.
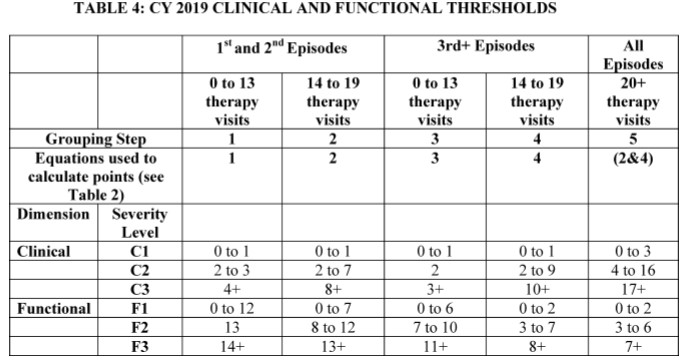
Functional Impairment Level (From OASIS)
- 30-day periods are categorized into one of three functional impairment levels.
- Certain OASIS items are used to create the functional impairment levels.
Steps for Creating the Functional Impairment Levels
- Determine points for response groups. Resource use is regressed on the seven OASIS items (along with other covariates from each of the PDGM groups). Regression coefficients determine the number of points. Points reflect relative resource group (high intensity, greater number of points).
- Calculate the functional score. For each 30-day period, points are summed to determine an overall functional score.
- Assign functional impairment level using score. Within each PDGM diagnosis grouping, periods are split into thirds and assigned to a low, medium, or high functional impairment group.
Select one of the following functional impairment levels to simulate a low, medium, or high PDGM diagnosis grouping HHRG.

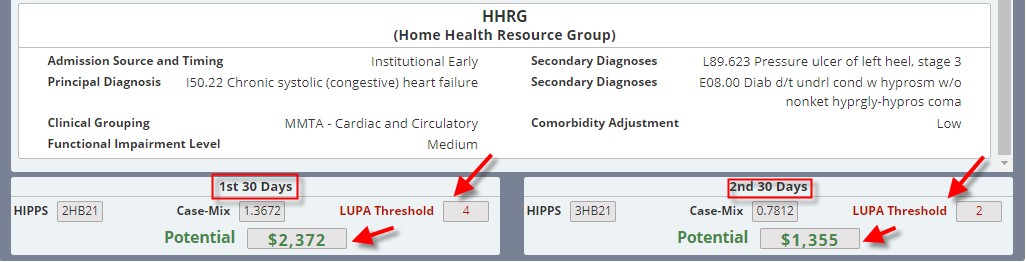
Home Health Resource Group (HHRG)
The Home Health Resource Group is comprised of five main case-mix variables:
- Admission Source
- Timing
- Clinical Grouping
- Functional Impairment Level
- Comorbidity Adjustment
A 30-day period is grouped into one subcategory in each color category. This results in 432 possible case-mix adjusted payment groups into which a 30-day period can be placed:
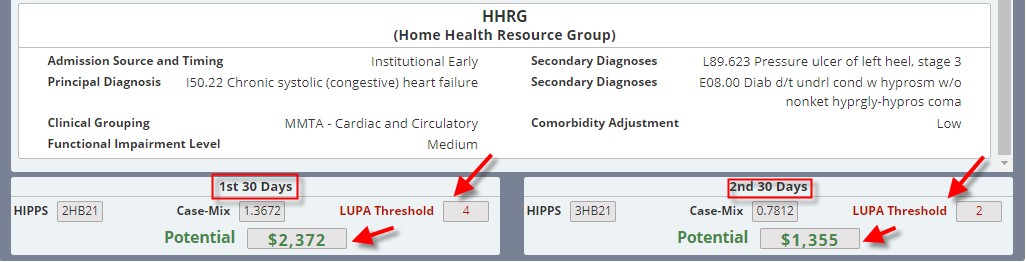
To select other responses for a new case-mix, simply start entering different information for each section.
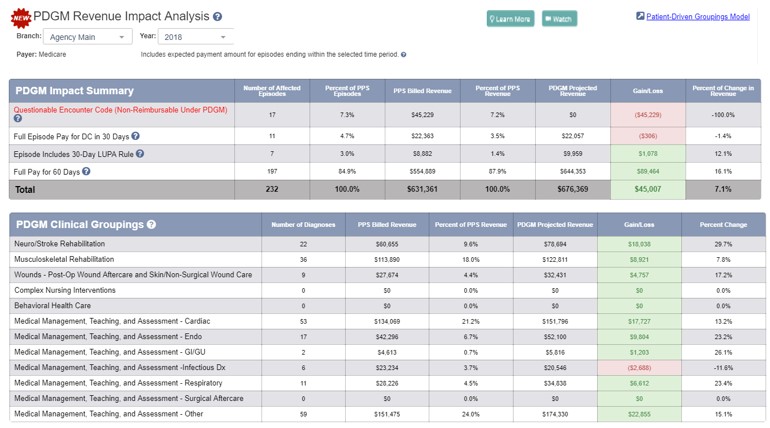
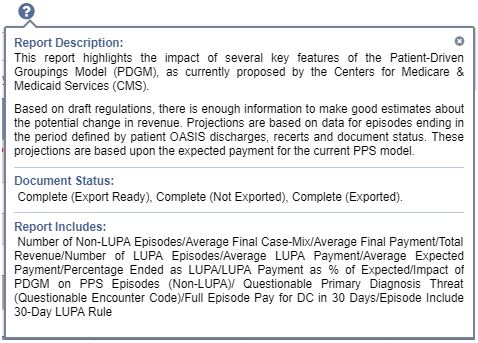
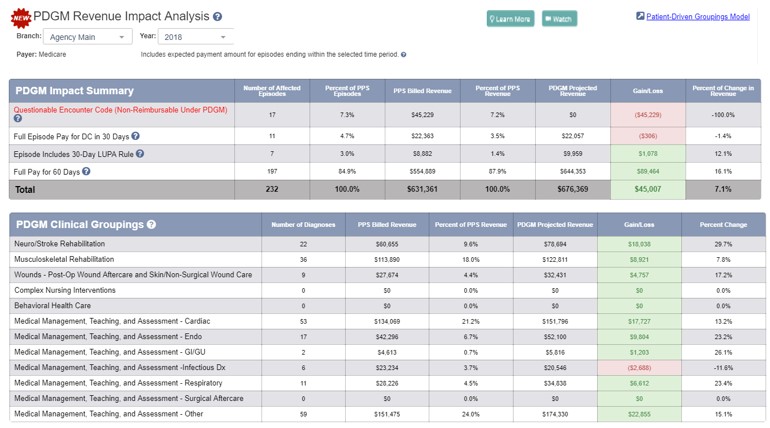
PDGM Revenue Impact Analysis
Using historical OASIS and visit information, this analysis assesses the impact of PDGM on revenue, based on past episodes. This data is more accurate than any comparable revenue impact analysis in the industry, since it assesses your data for the last three years and shows questionable encounter codes that will not generate payment under PDGM.
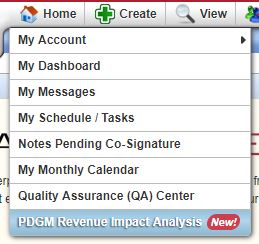
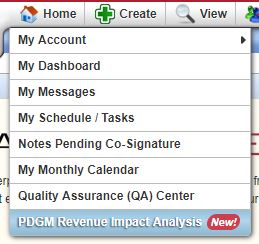
Accessing the PDGM Revenue Impact Analysis: Users with permission to view financial reporting can find this report under the Home or Reports tab.
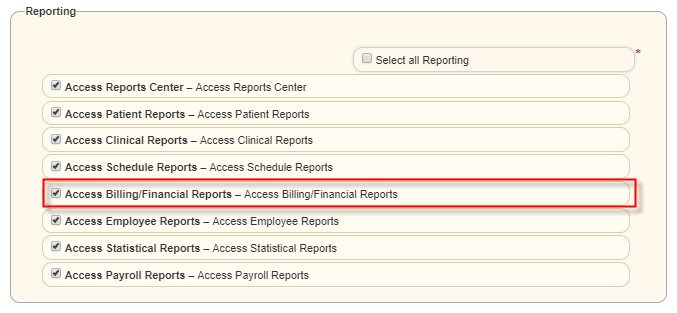
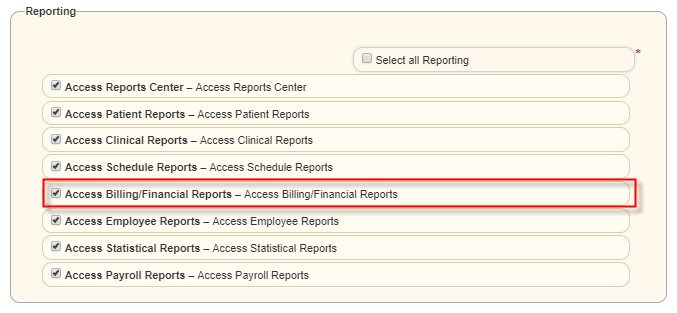
To give a user this permission, select the Admin tab> Lists > Users. In the Users list, find the appropriate user and select Edit. Select the Permissions tab on the left-side menu. Scroll to the Reporting section of the Permissions screen, and select Access Billing/Financial Reports. Click Save.
The user will then be able to view the PDGM Revenue Impact Analysis in the following locations.
From the Home tab:
From the Reports tab:

As you review your report, it will be immediately apparent how the questionable primary diagnosis encounter codes (which are not payable under PDGM) will financially impact your business. Preparing for these coding practices will have the greatest impact toward achieving success under PDGM.
There are multiple tool tips included in the report to guide you through the information.
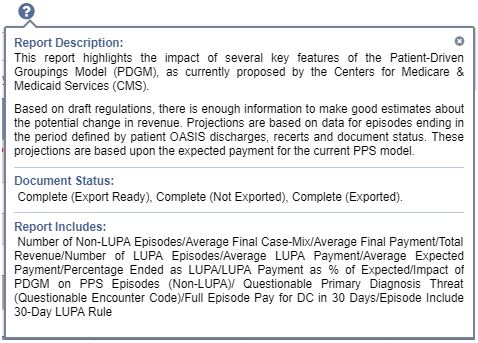
Included Episodes
- The report looks at the expected payment amounts for episodes within the selected year chosen for patients with an OASIS Discharge, Recertification, Resumption of Care, Transfer to Inpatient Facility, or Transfer Discharge.
- The report does not include sequestration, outliers, or Value-Based Purchasing adjustments.
- Information is available to review for 2017 and 2018. Information for 2019 includes financial data as of the last updated date, which is adjusted at the beginning of each month.

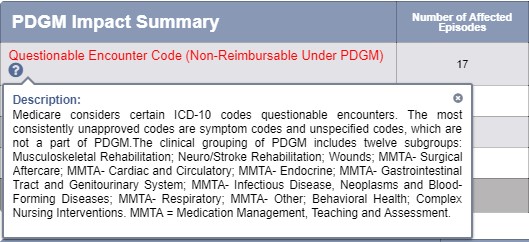
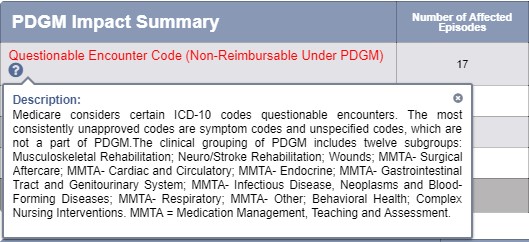
Questionable Episodes
The Questionable Encounter Code metric:
- Includes the number of affected episodes within the total number of episodes the agency has billed for the reporting period.
- Includes the percentage and number of questionable episodes where primary diagnosis codes that are not groupable under PDGM were used.
- Identifies how much revenue was billed under the current PPS billing system using questionable primary diagnosis codes and the dollar amount reflecting codes that will not be billable in January 2020 under PDGM.
Questionable episodes identify the greatest impact to the business and represent the greatest need for change to be financially successful under PDGM.
- ICD-10 codes that are symptom codes, R-codes, and codes with a description containing the phrase “unspecified” fall into the category of questionable episodes.
- See the PDGM Modeling Tool (Home tab>PDGM Modeling Tool) to learn more about the PDGM diagnosis impact upon billing.
- AgencyCore gives a warning when questionable codes are entered into the system at intake and on completion of the OASIS assessment.
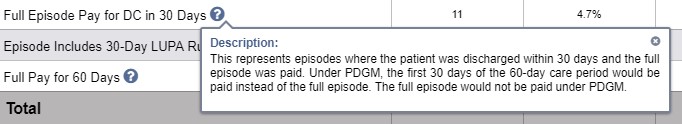
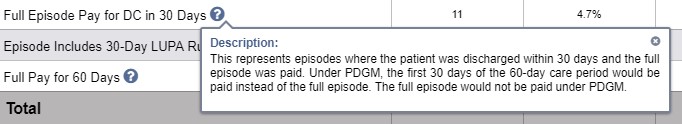
Full Episode Pay for DC in 30 Days
The Full Episode Pay for DC in 30 Days metric:
- Identifies episodes where the patient was discharged within 30 days, but the agency was paid for the entire 60-day episode.
- Includes the number of affected episodes within the total number of episodes the agency has billed for the reporting period.
- Includes the percentage of PPS episodes and the amount or revenue billed.
- The PDGM projected revenue is calculated based upon the new 30-day payment episode as the full 60-day payment episode will not be paid under PDGM.
- The gain/loss of patients discharged while the agency received full payment for the 60-day episode, and the percent of change in revenue, enables agencies to evaluate financial impact.
- Under PDGM, if a patient is discharged from care during the first 30-day payment period, there is no payment for the second pay period.
- If the number of visits provided in the first 30 days meets the LUPA threshold for that period, a full payment is provided for the first payment period.
- For episodes that begin with a Start of Care, the payment will be approximately 85% of what it would have been paid for the full episode under PPS.
- For episodes that begin with a Recertification, the payment for the first payment period will be about half of what would have been paid under PPS for equal work.
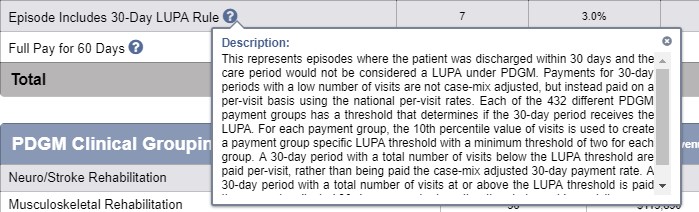
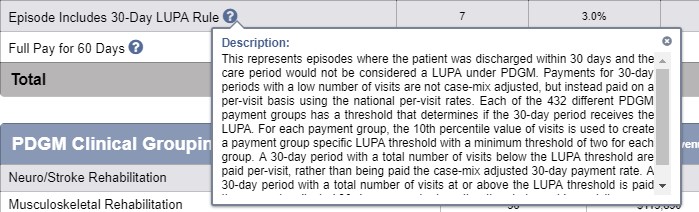
Episode Includes 30-Day LUPA Rule
- LUPAs under PDGM are more vital than before.
- LUPA rates vary and are based upon 30-day pay periods (versus 60-day pay periods under PPS).
- Under PDGM, each of the 436 HHRGs has an assigned LUPA threshold.
- The value of these thresholds varies from 2 to 6 visits.
- If the visits provided in a 30-day payment period do not meet the threshold, payment will be based on a per visit rate (no change from PPS).
- One or both payment periods can be paid on a per visit basis. The percentage of episodes with a LUPA portion may be higher than experienced under PPS.
- Overall, Axxess clients have an average of 14% of episodes containing at least one LUPA payment period. In comparison, about 9% of the episodes were treated as LUPAs under PDGM.
- AgencyCore identifies LUPAs for each 30-day payment period in the PDGM Case-Mix Analysis Report.
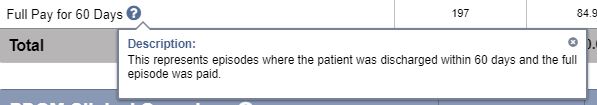
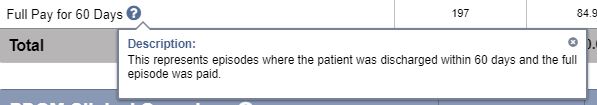
Full Pay for 60 Days
- The Full Pay for 60 Days metric identifies episodes where the patient was discharged by the end of the 60-day payment episode and the full episode was paid.
- Generally, this happens with about half of the episodes provided by an agency and the sum of the payments for the two payment periods is about 15% higher than the payment received under PPS.
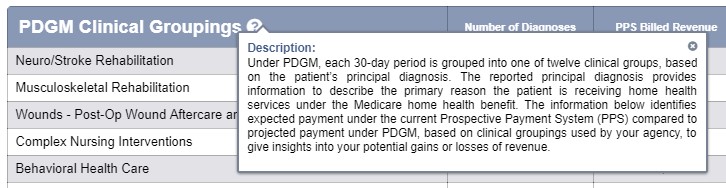
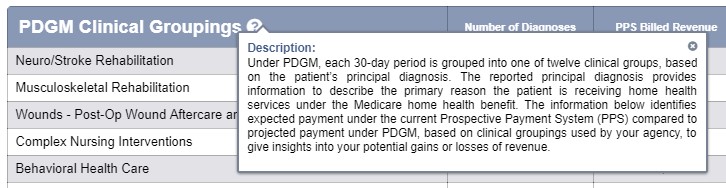
PDGM Clinical Groupings
- This section identifies diagnosis types commonly used by your agency and the corresponding clinical groupings.
- Questionable encounter codes are not listed in the Clinical Groupings, since they are not groupable.
Cost Modeling
- The visits for each discipline are based on the visit frequency entered by the clinician in the OASIS assessment. If M2200 is greater than zero, the therapy visits will need to be readjusted according to your agency policies and procedures, since most clinicians write a frequency of 1w1 for evaluation and treatment.
- If the case-mix analysis does not support the number of visits requested by the clinician, the frequency may be adjusted here, and then must be corrected in the OASIS assessment to ensure the Plan of Care is updated.
- The frequency times the average cost per discipline plus the supplies equals the total cost of the patient’s care.
Frequency X Average Cost Per Discipline + Supplies = Total Cost
The average cost per discipline is pulled from Manage Company Information and should be based on numbers from the agency’s cost report, which includes visit cost plus overhead.
- Non-routine supplies (NRS) are included in the expected payment. The supplies field available in Cost Modeling gives the ability to add additional supply expenses to the total cost.
- Anytime the Gross Margin Calculator is reopened, the information is automatically refreshed with data that is currently in the OASIS assessment.
Payment Projection
- The case-mix rate is adjusted when the therapy visits are adjusted in the Cost Modeling section, when there are outliers or LUPAs (based on the number of discipline visits) and when the OASIS items are corrected in the assessment.
- Anytime the Gross Margin Calculator is reopened, the information is automatically refreshed with data that is currently in the OASIS assessment.
- When the Gross Margin Calculator is first opened, the expected payment, total cost and gross profit (margin) represent what was generated by the OASIS assessment. When adjustments are made in the Cost Modeling section, the adjusted expected payment, total cost, and gross profit/loss and gross margin will be reflected here.
- The expected payment is based upon the case-mix rate minus the total cost.
Case-Mix Rate – Total Cost = Expected Payment
OASIS Case-Mix Analysis
- Case-mix information is based on the completed OASIS assessment Reviewing the case-mix in relation to the HHRG allows agencies to take a closer look at utilization.
- The case-mix analysis includes the following sections: Clinical Points, Functional Points and Non-Routine Supplies (NRS) Points.
Clinical Points:
- Based on the PPS calculation.
- Includes case-mix diagnoses entered in M1021 and M1023, and selected OASIS items based on episode sequence and therapy utilization.
- Other OASIS items that are part of the case-mix based on episode sequence and therapy utilization include:
- M1030- Therapy at Home response 1, 2 or 3
- M1200- Vision response 1 or more
- M1242- Pain response 3 or 4
- M1311- 2 or more pressure ulcers at stage 3 or 4
- M1324- Most problematic pressure ulcer response 1, 2, 3 or 4
- M1334- Stasis ulcer status response 2 or 3
- M1342- Surgical wound status response 2 or 3
- M1400- Dyspnea response 2, 3, or 4
- M1620- Bowel Incontinence response 2 through 5
- M1630- Ostomy response 1 or 2
- M20230- Injectable Drug Use does not produce points in the case-mix
Functional Points:
- Based on the PPS calculation for the following OASIS items:
- M1810 or M1820- Dressing upper or lower body response 1, 2 or 3
- M1830- Bathing response 2 or greater
- M1840- Toileting transferring response 2 or more
- M1850- Transferring response 2 or more
- M1860- Ambulation response 1, 2, 3 or 4
Non-Routine Supplies (NRS) Points:
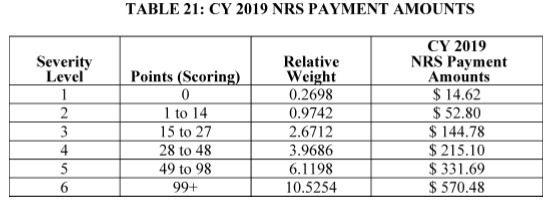
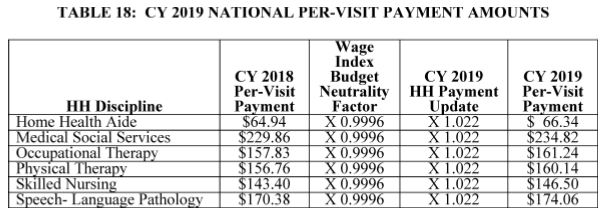
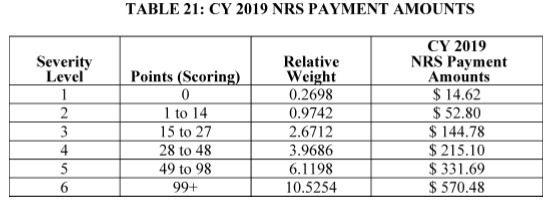
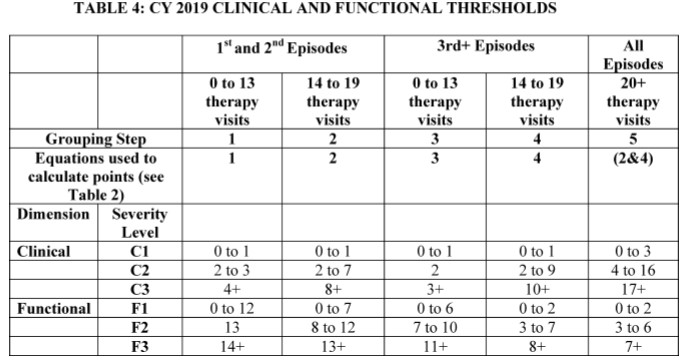
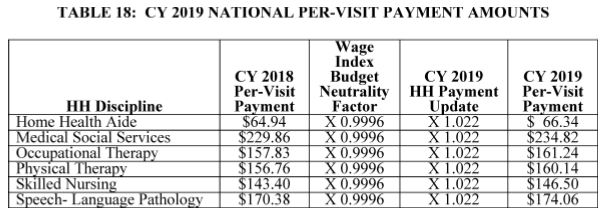
The table below demonstrates the total points for the corresponding therapy visits and episode that produce the Home Health Resource Group (HHRG):
Intake Form Updates
During the intake process, alerts notify you instantly if a diagnosis is payable under PDGM, so you know immediately if more information is required to generate a payable code. This system enhancement enables you to decide at intake if a patient is eligible for home health services, and protects your revenue for the care your agency provides.
An overview of updates made to the intake forms in preparation for PDGM is provided below:
Demographics Tab
Admission Source and Timing have been added to the intake process in preparation for PDGM. It is vital that this information is entered into the system correctly. This information will be the basis of several reports and PDGM projection tools at intake.
The information entered here will flow to the OASIS assessment.
Clinical/Diagnoses Tab
Primary Diagnosis is now required in Axxess AgencyCore.
- When a questionable encounter code is entered in the Primary Diagnosis field, a message will appear to alert the user that the diagnosis is not payable under PDGM (effective January 2020).
- Questionable encounter codes (including R-codes and unspecific codes) present the greatest threat to your agency’s revenue under PDGM.
- When your agency receives a questionable encounter diagnosis code, query the referring physician for more specific information, to identify a more appropriate diagnosis code under PDGM and update the face-to-face information.
- If the patient’s insurance group will not be impacted by PDGM, you can clear the warning message and proceed. Clear the warning message by clicking the “x” in the top right corner.
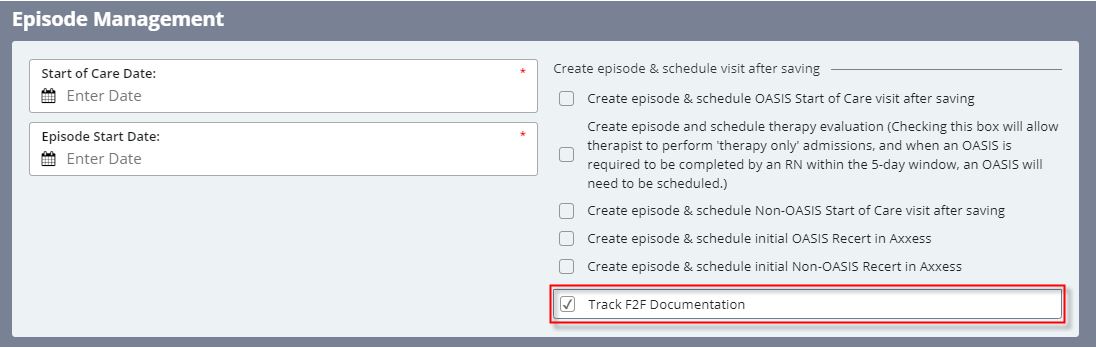
Referral Tab
Selecting a face-to-face encounter option is now required in AgencyCore. For insurance types that require a face-to-face encounter visit (e.g., Medicare, Medicaid), the date of the physician encounter is required as a part of the certification statement on the Plan of Care. Two responses are available:
- Date of Face-to-Face Visit
- Select when the physician encounter documentation for the primary diagnosis has been received. The date will flow to the Plan of Care to ensure compliance for certification.
- Face-to-Face to be Completed Within 30 Days
- Select when the face-to-face information is not available.
- Select to track the face-to-face information on the Demographics tab.
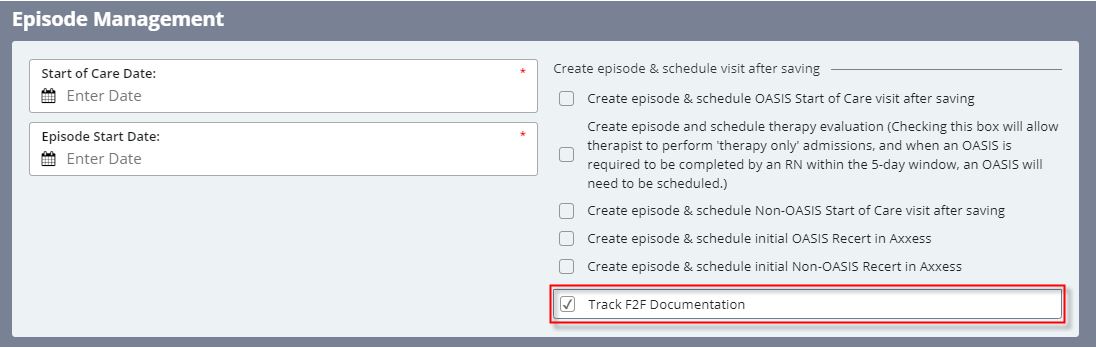
- Once the face-to-face documentation is received from the physician, enter the date: Patient Charts > Edit > Referral Information > Face-to-Face Evaluation Information > Enter Date of Face-to-Face
- The date will flow to the Plan of Care and can be sent to the physician for signature. Remember that payment will not be provided without face-to-face visit documentation, under PDGM.
A third response option (N/A) is available when face-to-face documentation is not required by the insurance payer.
Tool tips provide additional information and resources for understanding face-to-face regulations.