

With billing permissions, you will have the ability to access the billing center located on the AgencyCore Menu bar as well as have the Outstanding Claims dashboard panel.
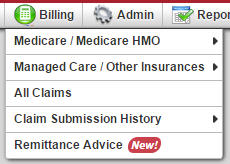 The Billing Menu contains five main categories:
The Billing Menu contains five main categories:
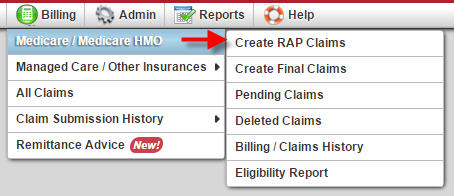 The Medicare/Medicare HMO menu category contains six sub menus. These menu items provide you the ability to create and manage your agency’s Medicare and Medicare HMO claims. When a Medicare or Medicare HMO patient is admitted AgencyCore automatically creates a RAP and Final claim for the patient. Axxess will submit EDI paperwork on behalf of your agency, which will allow for electronic claim submission to Medicare directly from AgencyCore. This eliminates the process of batching and uploading claims into DDE from applications such as Ability. Axxess provides the option to batch and bill Medicare claims while awaiting EDI processing from the intermediary. Medicare HMO RAP’s may be billed electronically through Availity, (a clearinghouse Axxess uses to bill non-Medicare payors), clearing house upload, mailing paper claims or direct entry into the HMO’s website if available.
The Medicare/Medicare HMO menu category contains six sub menus. These menu items provide you the ability to create and manage your agency’s Medicare and Medicare HMO claims. When a Medicare or Medicare HMO patient is admitted AgencyCore automatically creates a RAP and Final claim for the patient. Axxess will submit EDI paperwork on behalf of your agency, which will allow for electronic claim submission to Medicare directly from AgencyCore. This eliminates the process of batching and uploading claims into DDE from applications such as Ability. Axxess provides the option to batch and bill Medicare claims while awaiting EDI processing from the intermediary. Medicare HMO RAP’s may be billed electronically through Availity, (a clearinghouse Axxess uses to bill non-Medicare payors), clearing house upload, mailing paper claims or direct entry into the HMO’s website if available.
Create RAP Claims allows you to generate RAP claims for both Medicare and Medicare HMO payors. Three requirements must be met in order for AgencyCore to allow the generation of a RAP claim. The requirements are:
Similar to the create RAP claims menu item the Create Final Claims menu provides the avenue to bill episode final claims to the respective episodic payor, be it Medicare or a Medicare HMO. The Create Final Claims menu contains four edits that a claim must pass in order to be submitted for payment. The edits/requirements are:
Once all requirements are met you can generate the claim to the payor. Once a Medicare/Medicare HMO claim is submitted to the payor it moves to the Pending Claims menu. This menu allows for tracking of claim payment.
The Billing/Claims History menu contains all claim history information for a patient. This includes the ability to:
In addition, you can create a new RAP or Final claim in the Billing/Claims History view.
The Eligibility Report allows quick access to view all the eligibility reports for a patient. Axxess completes eligibility checks automatically every two weeks.
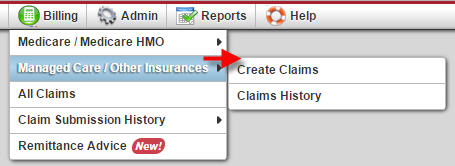 The Managed Care/Other Insurances category contains two sub-menus. Unlike Medicare/Medicare HMO payors, you must manually add claims for patients who have a managed care/other insurance payor through the Claims History option.
The Managed Care/Other Insurances category contains two sub-menus. Unlike Medicare/Medicare HMO payors, you must manually add claims for patients who have a managed care/other insurance payor through the Claims History option.
Once a claim is added through the claims history menu it will be displayed in the Create Claims menu until the claim is created/generated to the payor. Prior to generating a claim to a payor you must review and validate four items
Once the items are verified the claim is available for generation. You may choose to use Availity for electronic submission, clearing house upload, mail paper claims or key directly into an insurance portal. Choices may depend on payor requirements and/or agency preference.
The Claims History Menu is used to view and update Managed Care/Other Insurance claims. Features include the ability to add new claim time frames, view payment history, post payments and adjustments, view the invoice in the UB04, HCFA 1500 or invoice format as well as claim deletion.
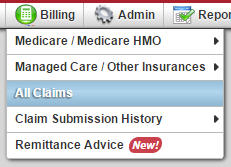 The All Claims allows you to view all claims by payor to complete verification and submission of claims.
The All Claims allows you to view all claims by payor to complete verification and submission of claims.
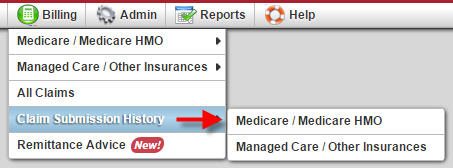 Claims Submission History shows submission date, batch number, patients included in batch under view claims and responses from submitted claims. This section has two sub-sections; Medicare / Medicare HMO and Managed Care / Other Insurances.
Claims Submission History shows submission date, batch number, patients included in batch under view claims and responses from submitted claims. This section has two sub-sections; Medicare / Medicare HMO and Managed Care / Other Insurances.
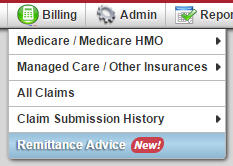 The Remittance Advice menu lists all Medicare remittances for your agency. The default view is set to the prior two months. You do have the ability to view the remittance details and quickly post payments. The remittance advice includes items such as the claim status, payment amount, any adjustments and bill type. This section now allows you to view Remits for Medicare / Medicare HMO as well as Managed Care / Other Insurances.
The Remittance Advice menu lists all Medicare remittances for your agency. The default view is set to the prior two months. You do have the ability to view the remittance details and quickly post payments. The remittance advice includes items such as the claim status, payment amount, any adjustments and bill type. This section now allows you to view Remits for Medicare / Medicare HMO as well as Managed Care / Other Insurances.