

AgencyCore is connected to the CMS/Medicare database and utilizes the Patient’s demographic data which has been input to check and verify the Medicare Eligibility of the specific Patient.
If you are currently downloading your claim files, You may continue to do so. Sending the claims directly from AgencyCore to your clearinghouse or Medicare fiscal intermediary is a lot easier.
Yes. You can submit electronic claims to any clearinghouse that accepts such claim files.
Yes, you can submit claims electronically through AgencyCore. If your insurance provider or clearing house accepts electronic claims, the claim files can be generated from Axxess’ AgencyCore.
For Medicare patients, claims can be electronically submitted to your Regional Home Health Intermediary like Palmetto, Cigna, NGS or Anthem. Claims can also be submitted to other Part A and Part B clearinghouses.
For Private Insurance, you can submit electronically as well. We submit claims to Zirmed, Availity, Emdeon and other clearing houses.
For more information, visit the Submit Electronic Claims tutorial. Please contact our office at (866)795-5590, and one of our representatives will assist you.
For most insurance providers, the process is quick. If you are already enrolled with the insurance provider to submit claims electronically, you will be able to do so from within Axxess’ AgencyCore almost immediately.
If you aren’t already enrolled with your insurance provider to submit claims electronically, for Medicare claims, it normally takes 4-6 weeks for Medicare to receive and process the application. Once this has been done, you will be able to submit claims electronically as well as receive your remittance advice electronically.
You can bill any insurance company. You can find more information in the Insurance / Payor Information tutorial. However, in short to add a new insurance:
You can submit a batch of claims. To do so, complete the RAP/final (EOE) verification process and select Generate all Completed. A list of all verified claims will appear, then select Submit Electronically. You can find more details on submitting claims in the Managed Care / Other Insurances and Medicare / Medicare HMO sections of the AgencyCore tutorials.
More details found in the Pending Claim tutorial, but in short.
NOTE: The Pending Claims show you claims that have been submitted already. You can update the payment status to remove the claims from the list.
You can generate claim cancellations from AgencyCore. You can also cancel the claims in the Medicare DDE system other tools provided by your clearinghouse.
You can submit a RAP after the OASIS SOC or Recertification OASIS and the first billable visit has been completed.
If the changes made affect the date or the HHRG, then you will need to submit those changes so that they reflect on the RAP.
Yes, HHRG groupers are used to calculate the prospective payment for the episode.
HIPPS is a Medicare acronym for Health Insurance Prospective Payment System (HIPPS). A HIPPS code is generated after an OASIS assessment is completed. The HIPPS code determines the prospective payment for the episode.
Make sure you have answered M2200 in the OASIS assessment. If no therapy is needed you must place three zeros in the field provided. (ex. 000)
If this does not fix the problem, please call Axxess’ office and one of our representatives will assist you.
This acronym stands for Healthcare Common Procedure Coding System.
HCPCS codes are used to identify the discipline you are billing for.
HCPCS codes are determined by your payment intermediary or Insurance Provider.
For Medicare claims and visits, Axxess’ AgencyCore automatically assigns the proper G Code associated with the task/document. For other insurances, you have the option to specify the HCPCS codes required by the insurance company.
It is not necessary to look up the G Codes. The G Codes are established based on the type of visit scheduled. (ex: SN Visit – G0154)
Yes, AgencyCore includes DME billing in the patient chart, and for RAPs and Final billing submissions.
Modifiers are claim enhancers used to specify multiple services within the same episode.
Yes, you can bill Managed Care, Medicare, Medicare Replacement plans, HMO’S, Private insurance and Medicaid through AgencyCore.
Yes. When you go into OASIS Export from the Create tab, click on the drop-down menu beside Payment Source. Select which insurance companies you want to submit an OASIS, then click Generate.
Go into OASIS Export from the Create tab, click on the drop-down menu beside Payment Source. Select which insurance companies you want to submit an OASIS, then click Generate. Click the box beside the OASIS assessments to select the assessments you want to submit. Click on Generate OASIS file at the bottom. Save to your computer, then go to your ATT or Verizon dialer and upload.
The RAP and Final (EOE) both have a verification process that must be completed before processing your claim. This verification process helps to prevent data errors that may cause a claim to reject or go into correction status.
No. You may need such a service to submit your OASIS assessments or to maintain access to the Medicare DDE system.
Supplies can be added to each skilled nurse visit on the supply worksheet, or supplies can be added on your final (EOE) claim. You can learn more in the Supplies tutorial.
At the bottom of each progress note, there is an option to document the type and quantity of supplies used. Axxess’ AgencyCore automatically transfers that information for billing purposes. Users with Axxess to the billing portion can modify the supplies used accordingly before the claim is created.
EDI electronic submissions are submitted through a clearinghouse. Axxess’ AgencyCore allows you to submit claims directly to any clearinghouse that accepts electronic claims. If the insurance company only accepts paper claims, a UB-04 or HCFA 1500 claim form can be downloaded, printed and mailed directly to the insurance payor.
To obtain access to CMS DDE (Direct Data Entry) system, an EDI enrollment must be completed. After your enrollment process is complete, CMS will establish a username and password that is unique for your agency. Axxess will offer any assistance you need to help complete the enrollment process.
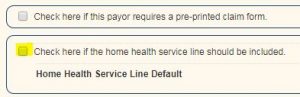
Make sure highlighted box is unchecked.
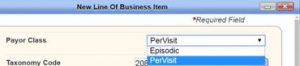
2. If the claim does not require a RAP or Final (EOE), change the Payor class from Episodic to Per-Visit by following the steps 1-3 on Number 1.
Please check the Patient’s listed Demographics
Created Next Episode
Please ensure that the “NEXT Episode” has been created if the client is having challenges with the RECERTIFICATION HIPPS/HHRG calculated amount not displaying.
The Episode Timing Must NOT be “NA”
Primary Diagnosis – Please ensure that the Primary DX code is reflective of the ICD-10 rules for services. The ICD-10 codes can be challenging with deeper levels of specificity and exceptions.
Therapy Need Must Not be “NA”
User Permission
Please make sure that their User “Permissions” have not been restricted or modified.
NON-Medicare “Payor Set-up”
Please make sure they review how that “Payor” is set-up especially for the HMOs that follow Medicare guidelines.
To print a blank HCFA 1500, on a pre-printed form go to VIEW → LIST → INSURANCE/PAYORS. Find the insurance in question and click EDIT.
On the first page, under INSURANCE/PAYOR DETAILS, find the Payor Class you want to change and on the far right-hand side click EDIT,
Put a check in the first checkbox, CHECK HERE IF THE PAYOR REQUIRES A PREPRINTED CLAIM FORM, then click SAVE & CLOSE.
If your claim has already been created you will need to delete it and recreate it to pull the changes in.