System updates have been made to enable agencies to efficiently bill providers with secondary identifiers (IDs).
To bill a provider with a secondary ID and its ID type:
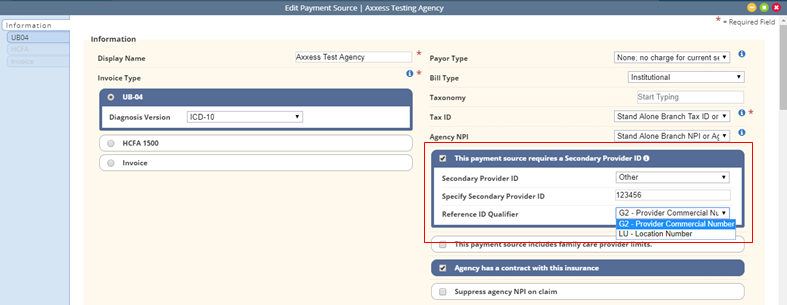
View tab ➜ Lists ➜ Payment Sources ➜ Edit ➜ Information tab ➜ This payment source requires a Secondary Provider ID
Select an option from the Secondary Provider ID drop-down menu. When Other is selected as the Secondary Provider ID, type the secondary provider ID in the Specify Secondary Provider ID field and select the appropriate Reference ID Qualifier.
To bill a provider with a secondary ID and its ID type at Claim or Service level:
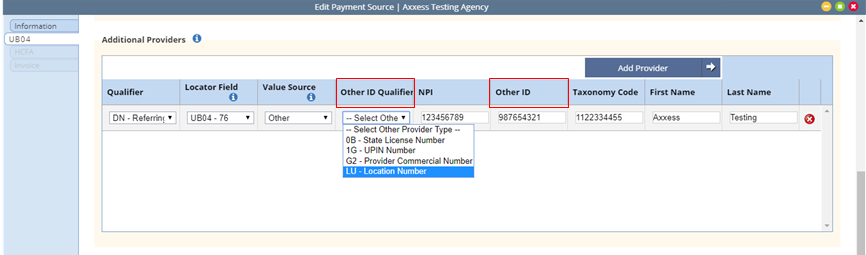
When Physician (Primary or Referral) or Clinician is selected as Value Source and Other ID Qualifier is specified, the Other ID is pulled from the following fields to populate the appropriate locations in the ANSI 837 file.
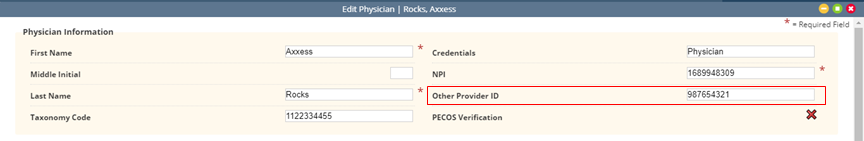
Physician:
View tab ➜ Lists ➜ Physicians ➜ Edit
In the Physician Information section, there is now an additional field for Other Provider ID.
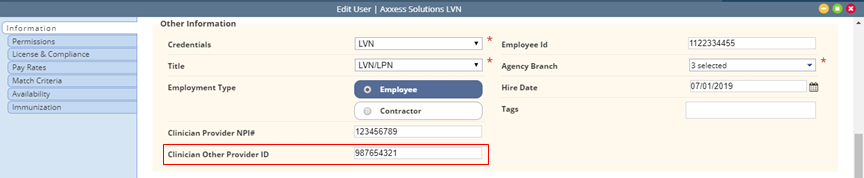
Clinician:
Employees tab ➜ Employee Center ➜ Edit
In the Other Information section of the Information tab, there is now an additional field for Clinician Other Provider ID.
Updated on 12/10/2019