Axxess Home Care now enables users to create claims based on authorizations set up for each payment source. By creating and processing claims according to specified authorizations, organizations can eliminate manual billing processes and streamline claims processing.
To set up authorizations for a new payment source, navigate to the Create tab and select Payment Source.
Create tab ➜ Payment Source
To set up authorizations for an existing payment source, navigate to the View tab, hover over Lists and select Payment Sources. Edit the payment source by selecting Edit under the Actions column.
View tab ➜ Lists ➜ Payment Sources ➜ Edit
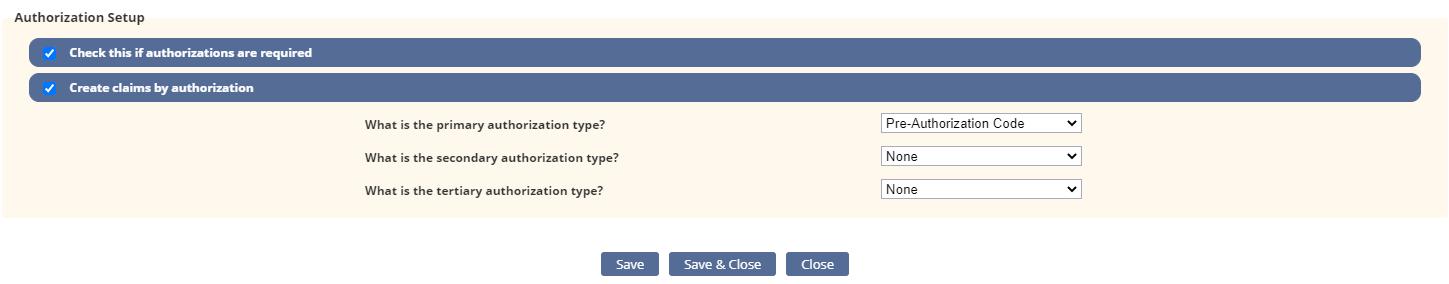
On the Information tab in the payment source setup, navigate to the Authorization Setup section. Select Check this if authorizations are required and Create claims by authorization. Click Save to complete the authorization setup process.
Once authorizations are set up for the appropriate payment sources, Axxess Home Care will create claims according to the authorizations entered. Authorizations include:
| The claim date range includes tasks that overlap authorization date ranges for the same services. | |
| The claim date range includes tasks that are associated with separate authorizations. | |
| The claim date range includes tasks that cover different authorized services and date ranges. |
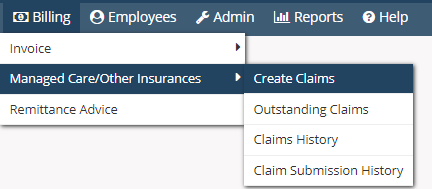
To create claims, navigate to Managed Care/Other Insurances under the Billing tab and select Create Claims.
Billing tab ➜ Managed Care/Other Insurances ➜ Create Claims
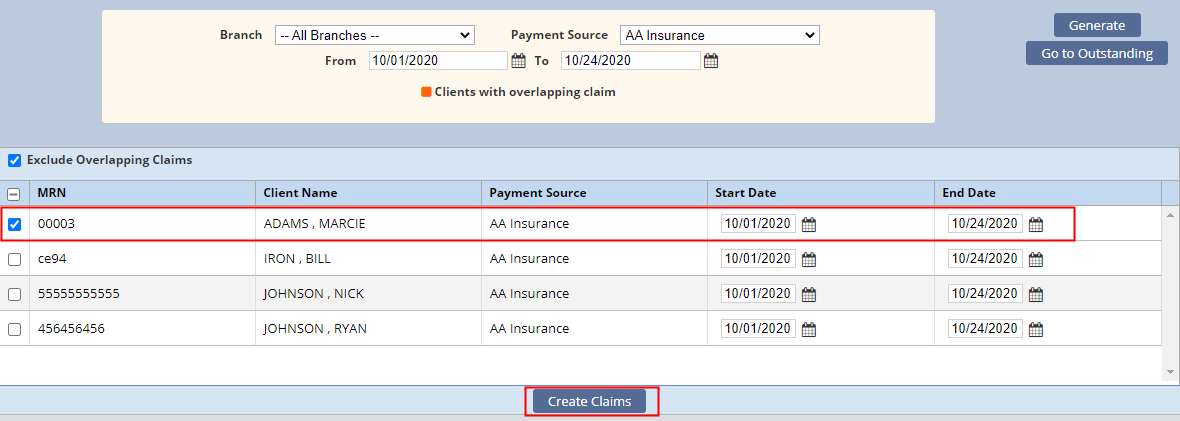
Enter the parameters at the top of the Create Claims screen and click Generate to generate a list of clients with claims to create.
Check the boxes next to claims you want to create and click Create Claims. The tasks will split into individual claims according to the authorizations identified for the payment source.
Once created, claims will appear on the Outstanding Claims screen.
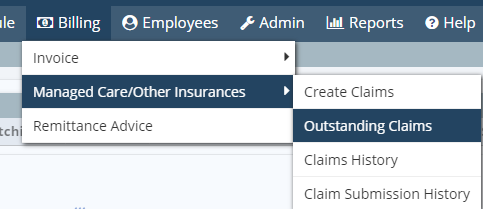
To view outstanding claims, navigate to Managed Care/Other Insurances under the Billing tab and select Outstanding Claims.
Billing tab ➜ Managed Care/Other Insurances ➜ Outstanding Claims
The claim information will appear according to the payment source’s authorizations. In the following example, the claim has been split into two line items for processing.
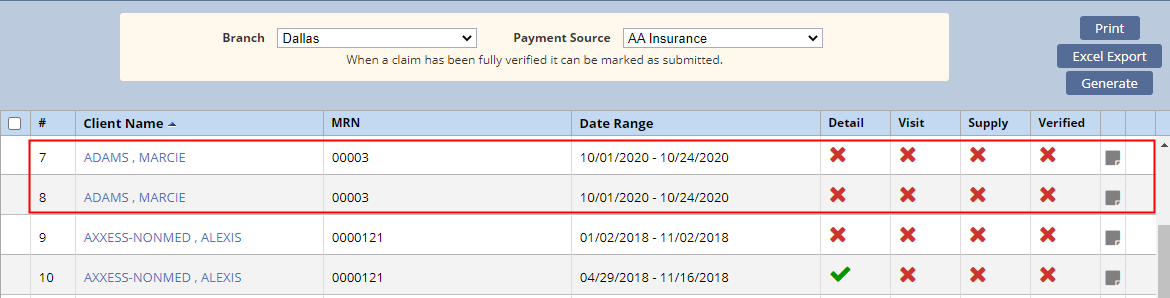
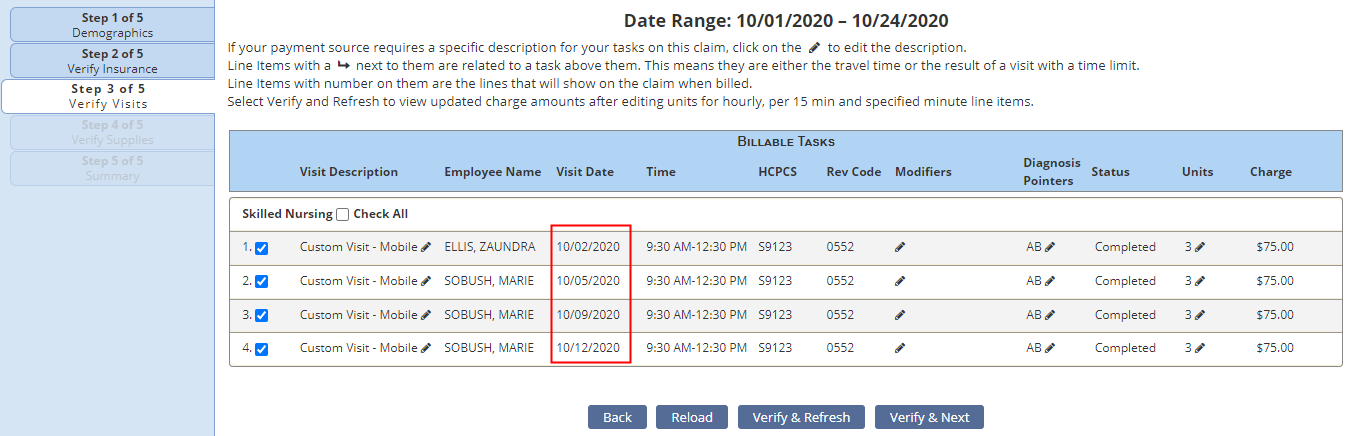
Select the client’s name to navigate to the claim verification screen, where you can view the service dates included in the claim. Visits included the two claims will correspond to the respective authorization dates.
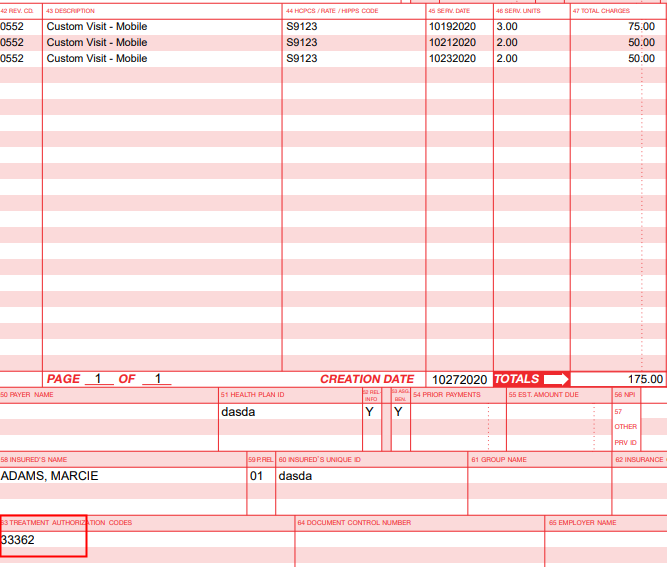
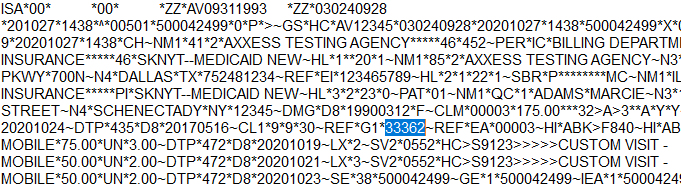
The associated authorization number will populate on the printed claim as well as the ANSI electronic file.
Updated on 10/28/2020