Axxess Palliative Care now provides a PHQ-9 depression screening that enables users to assess patients for depression using a standardized, evidence-based tool. This enhancement helps organizations track and monitor patients’ depression to improve patient care while staying compliant.
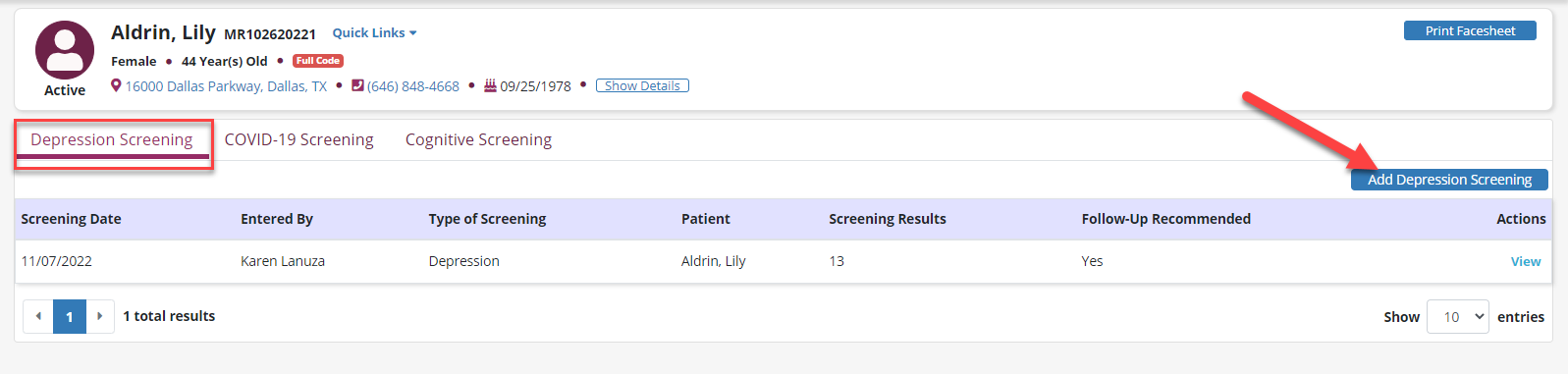
To document a depression screening for a patient, navigate to the Patients tab and select Screenings. On the Screenings page, stay on the Depression Screening tab and click Add Depression Screening.
Patients tab ➜ Screenings ➜ Depression Screening tab ➜ Add Depression Screening
Enter the start time for the depression screening. If your organization is engaged with MIPS quality measure 2v11, an algorithm will display to help you determine if a depression screening is necessary.
If your organization is not engaged with MIPS quality measures, or you would like to skip directly to administering the depression screening, click Administer Depression Screening. This will display the questions associated with the PHQ-9 evidence-based depression screening.
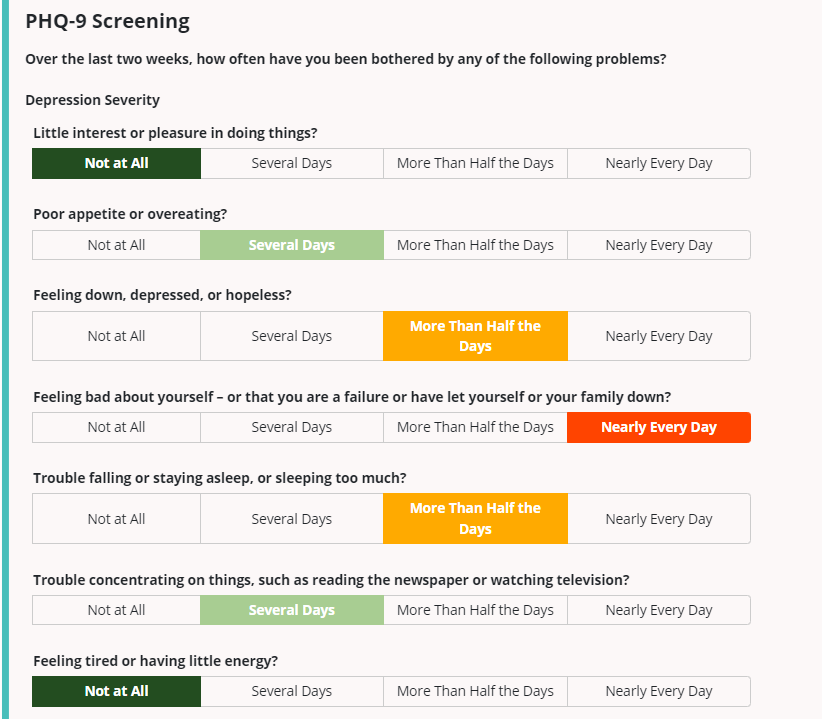
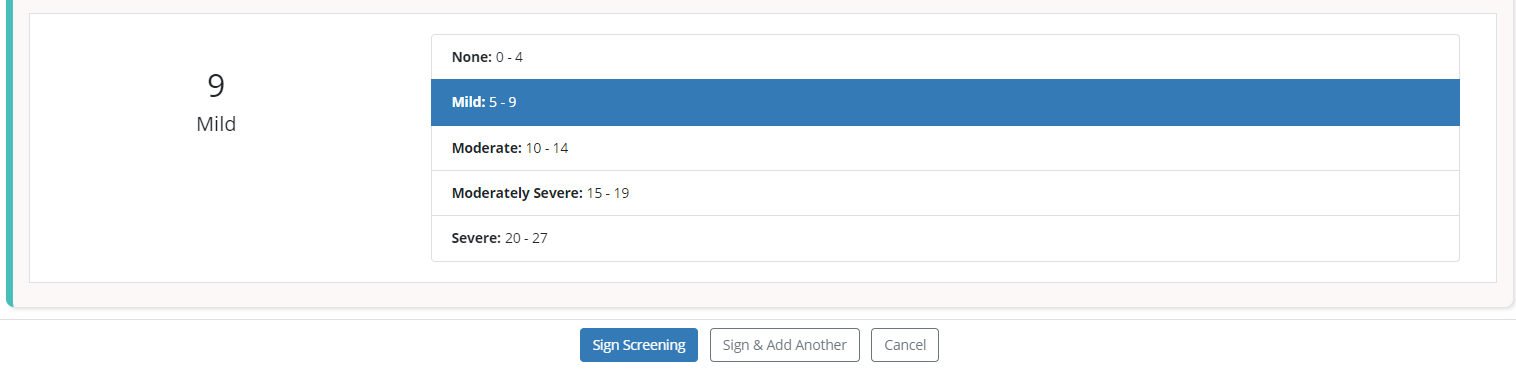
As you complete the PHQ-9 fields, the screening total will automatically calculate at the bottom of the screen.
When the screening is complete, select Sign Screening to save it to the patient’s chart.
Once a depression screening has been saved to the patient’s chart, users can view the screening by selecting View under Actions on the Depression Screening tab.
Patients tab ➜ Screenings ➜ Depression Screening tab ➜ Actions ➜ View
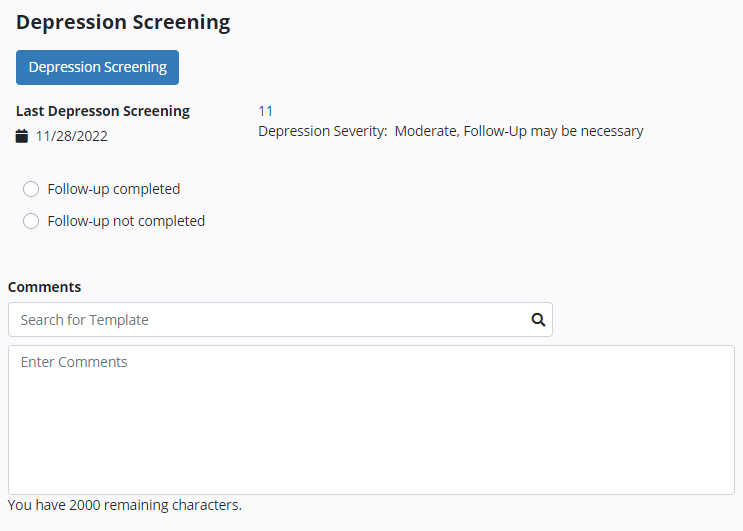
When documenting any visit with a Social/Emotional Assessment section, click the Depression Screening button to open the Depression Screening page and view past screenings or document a new screening.
This section also displays the date of the last depression screening, the results and whether or not a follow-up was indicated.
In this section, you can document a follow-up or the reason a follow-up was not completed. If your organization engages in MIPS quality measure 2v11, these documentation points will count toward your quality measure calculations.
Updated on 12/05/2022