Axxess Palliative Care now enables users to select applicable CPT codes when the Clinical Quality Measures (CQM) integration is enabled. CQM encompasses advance care planning, falls plan of care and elder maltreatment, which use CPT II codes (informational codes) on claims. By creating a workflow for calculation and CPT coding for organizations using these measures, this enhancement streamlines operations and improves quality measures.
To access this feature, the organization must enable the Clinical Quality Measures integration in Company Setup, activate at least one available measure in the patient’s environment and ensure users have access to clinical quality measure calculations.
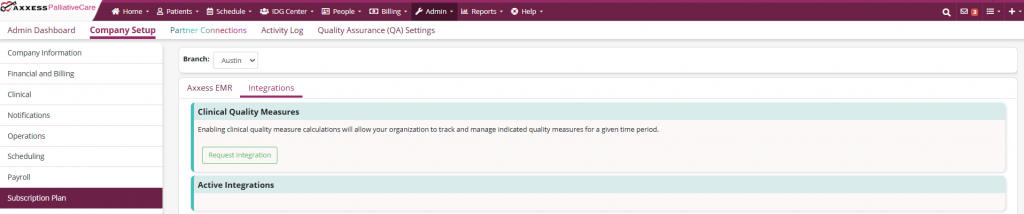
To activate the Clinical Quality Measures integration, the users with permission to view and edit Company Setup can navigate to the Admin tab and select Company Setup from the drop-down menu. On the Subscription tab, select Integrations and click Request Integration under the Clinical Quality Measures section.
Admin tab ➜ Company Setup ➜ Subscription tab ➜ Clinical Quality Measures section ➜ Request Integration
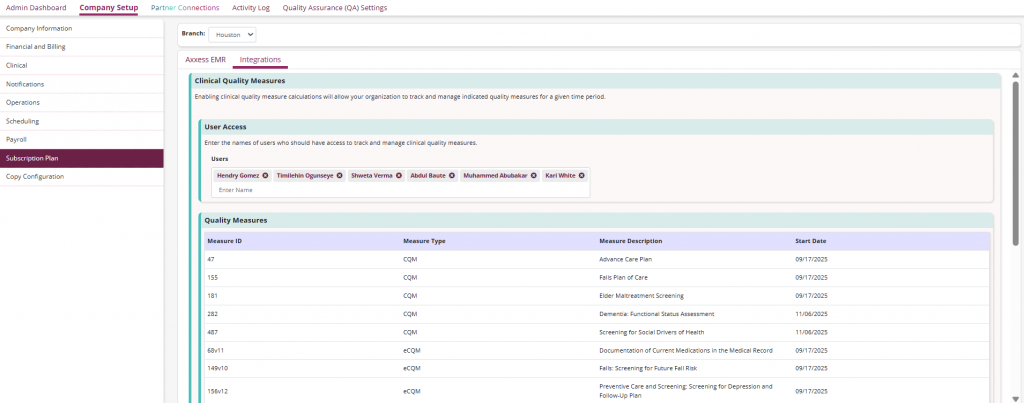
Once the integration is enabled in Company Setup, a User Access field will be accessible. In this field, the names of users tracking and managing clinical quality measures can be entered. A Quality Measures table will also be visible, this table displays the measures that have been enabled for the organization with the following columns: Measure ID, Measure Type, Measure Description and Start Date.
Once the visit is completed, the Clinical Quality Measures section will be displayed under Billing Codes.
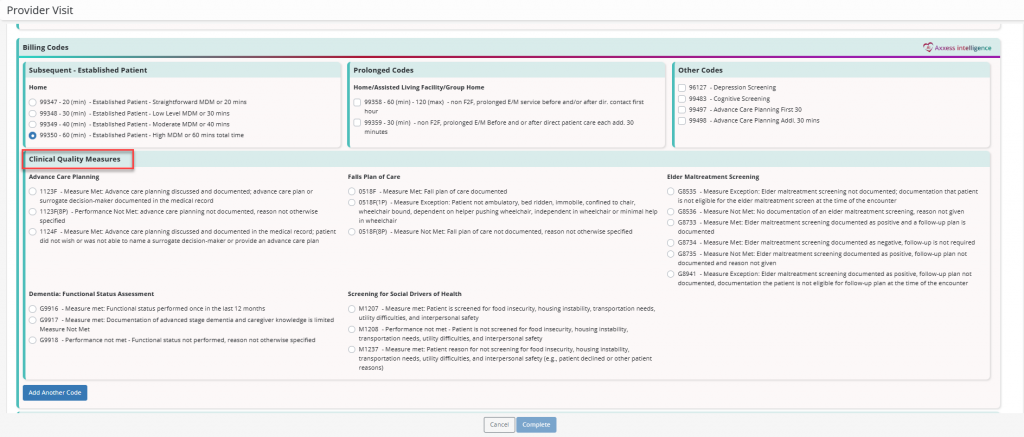
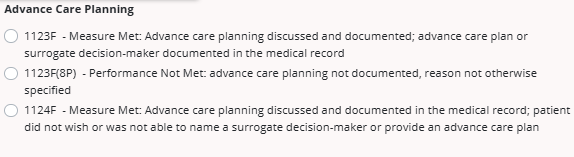
If the organization has advance care planning enabled in the integration, the Advance Care Planning section will appear with the following codes:
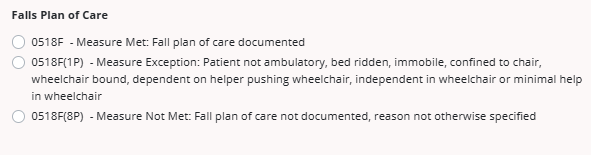
If the organization has falls plan of care enabled in the integration, the Falls Plan of Care section will appear with the following codes:
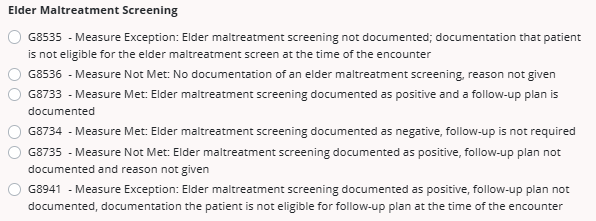
If the organization has elder maltreatment screening enabled in the integration, the Elder Maltreatment Screening section will appear with the following codes:
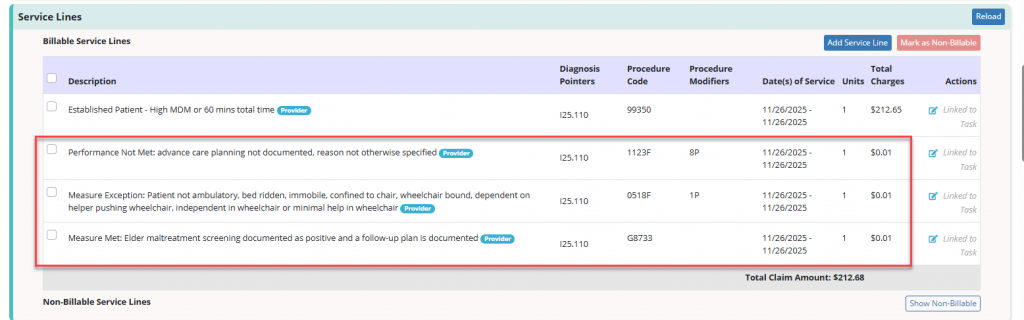
After a user completes a visit and selects the CQM codes, the corresponding CPT II codes will be displayed in the Billable Service Lines section when verifying a HCFA 1500 claim.
Updated on 12/03/2025