Checking a patient’s eligibility to receive services from an agency is essential to providing care. Navigate to the Eligibility tab in Axxess RCM to check eligibility and view details for existing eligibility requests.
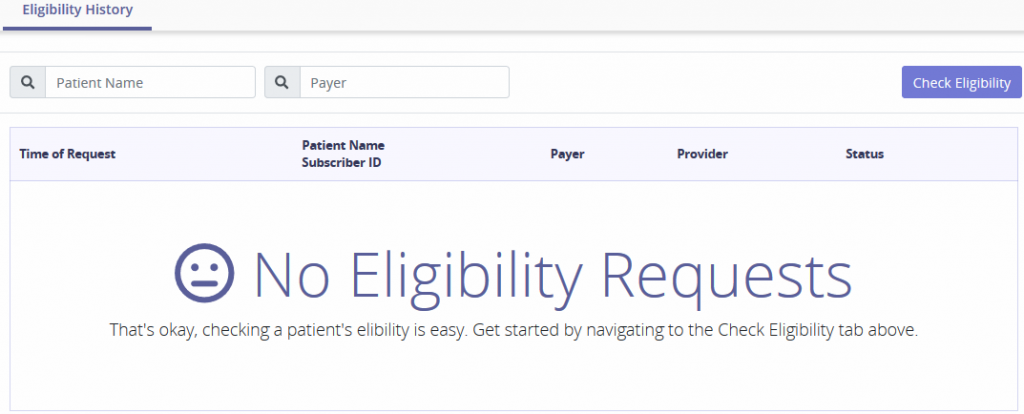
Search for eligibility requests by entering the Patient Name or Payer. The tab provides details of the Time of Request, Patient Name/Subscriber ID, Payer, Provider and Status of the request. If there are no requests, the following message will show:
Select the Check Eligibility button and the top of the screen to expand with the following form:
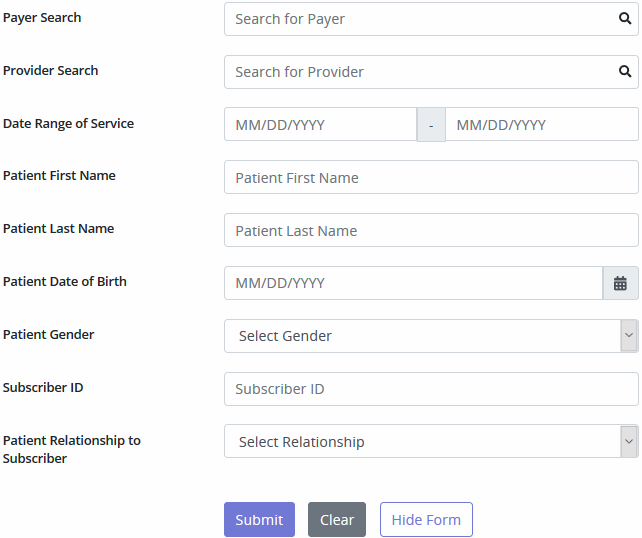
To generate a patient’s eligibility details, all sections must be completed.
Eligibility data will appear within 24 hours of the request. The Payer list will show all payers Axxess bills out to, even if Axxess is not assigned as the clearinghouse.
A message indicating Unknown Status will generate when the payer is not set up to support eligibility.