
One thing everyone in the home health industry can relate to is an environment of constant change. The Patient-Driven Groupings Model (PDGM) is only the latest example. There have been changes to ICD-10 codes and guidelines, CoPs, adjustments to the formatting of the OASIS, added and removed Outcomes and Process Measures, as well as reimbursement changes. The list goes on and on. Over the years, home health providers have faced many challenges and each time staff have to adapt to the change by planning, preparing and educating.
I often hear comments like this:
“We are finally grasping the current structure and learning how to manage effectively…now more change is thrown our way!?!”
It’s discouraging for providers when their purpose is to care for patients in the home, yet a great deal of time is spent on learning new rules and regulations. It’s no wonder staffing is a struggle in home health. We are all in this together, and with the sharing of information positive results can be achieved with planned actions. We are about to relearn, readjust and reset.
Understanding the HHRG
Under the Prospective Payment System (PPS), providers have become accustomed to the components of a Home Health Resource Group (HHRG) consisting of a clinical domain (C), functional domain (F) and service utilization domain (S). A score of C3F3S1, sheds light that the patient has high clinical and functional deficits and is within an early episode expecting 0-13 therapy visits. Under PPS there are 153 possible HHRGs.
Under the upcoming PDGM payment model, a case-mix adjusted payment for a 30-day period of care is made using one of 432 HHRGs. Each HHRG is represented as a Health Insurance Prospective Payment System (HIPPS) code on Medicare claims.
This diagram summarizes the case-mix system for PDGM.

Creating a PDGM HIPPS Code
According to the Medicare Claims Processing Change Request on February 1, 2019, the HHRG system above will be recorded on claims as HIPPS codes, using the following code structure:
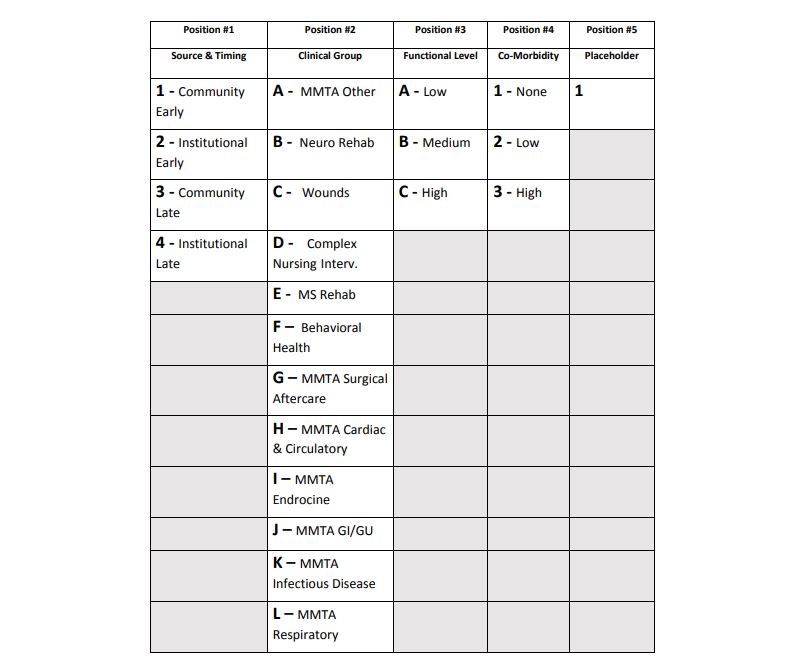
The distinct five position, alphanumeric home health HIPPS codes are created as follows:
- The first position remains a numeric value, but no longer represents a grouping step. The first position represents a combination of the referral source (community or institutional) and the period timing (early or late).
- The second and third positions continue to represent the clinical and functional domains of the HHRG coding system.
- The fourth position represents the comorbidity category that applies to the patient.
- The fifth position is a placeholder for future use, required only because the field used to report HIPPS codes requires five positions.
Using this structure, a second period for a patient with a hospital inpatient stay during the period, in the Wounds group, high functional severity and no comorbidity would be coded 4CC11.
HIPPS code rates represent specific characteristics (or case-mix) on which Medicare payment determinations are made. As with the HHRG under PPS, each HIPPS code has a corresponding case-mix weight. In the example listed above, 4CC11 has a case-mix of 1.5347.
Ensuring Compliance
Any home health provider that wishes to achieve growth in today’s marketplace must learn to master OASIS data accuracy and compliance. It is essential for providers to ensure they are receiving every penny they deserve based on the appropriate care provided to the patient. In addition, agencies must have the capability to analyze and manage their case-mix. A drop in the case-mix could result in the loss of hundreds to thousands of dollars for an agency.
Axxess has built features into our software that empower providers with data to manage case-mix and calculate the revenue impact of PDGM. These features enable education, visibility, and training for leaders and other staff to make changes now so they will be ready for PDGM. In addition to resources available online, Axxess is leading the way to train the industry on exactly what agencies should do to thrive when the new payment model takes effect. Registration at one of our interactive one-day seminars is open.
