
Often in reviewing clinical records, quality assurance (QA) staff look for items that are not a concern for surveyors or auditors.
Inconsistency, requests, and phone calls from QA while doing visits and interruptions when at home all add to the confusion surrounding documentation. The ambiguity behind reviews can lead to frustration for the clinical staff responsible for collecting data.
As we enter into value-based purchasing (VBP), it is important that home health staff be adequately trained on the Outcome and Assessment Information Set (OASIS), expected outcomes, Medicare policies and the Home Health Conditions of Participation. A robust orientation for every staff member should be provided by the organization to reduce time for QA staff and ease the frustration of clinical field staff.
What Should the Quality Assurance Staff Focus On?
- Assuring OASIS is well understood by QA staff and clinical staff is imperative to achieving VBP goals. This should be a top priority for every organization. Items in the M1800 series should be a specific target area. Be sure to include the M1700s in this training since the cognitive and behavior issues experienced by the patient can significantly impact mobility and ability to perform activities of daily living (ADLs) and instrumental activities of daily living (IADLs).
- Be certain the Medicare Benefit Policy Manual available for staff is the most up-to-date version. Review the coverage policies for Medicare. Therapy and social worker coverage is clearly outlined here. Therapists and social workers should be well versed in these policies and ensure the documentation reflects policy requirements.
- Nurses should spend time reviewing and understanding coverage areas in this manual. There are likely surprises to both nurses and QA Staff. The 15 clearly outlined areas of coverage will need to be well understood and documentation must reflect at least one of these 15 items as ordered within the physician’s plan of care.
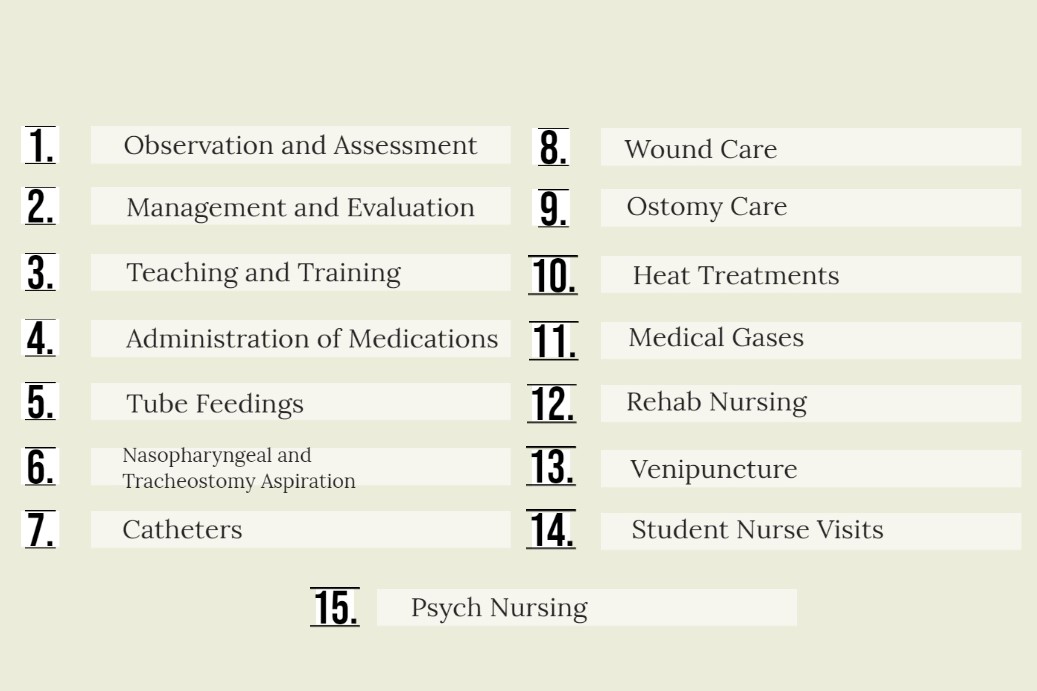
- It is important that each staff member completing skilled visits understands each of these coverage areas and what documentation items are necessary to satisfy compliance in each area. Audits by each Medicare Administrative Contractor (MAC), Recovery Audit Contractor (RAC) and others will expect full compliance.
- Nurses should spend time reviewing and understanding coverage areas in this manual. There are likely surprises to both nurses and QA Staff. The 15 clearly outlined areas of coverage will need to be well understood and documentation must reflect at least one of these 15 items as ordered within the physician’s plan of care.
- Orientation should include a complete training and knowledge assessment of the conditions of participation to help imprint required items. Documentation should show a strong understanding of these standards. Remember, surveyors will look for documentation reflecting all items necessary to satisfy every condition.
Gone are the days of the “Quality Assurance Department” calling for unimportant and trivial corrections to documentation submitted.
QA should look for compliance with OASIS, policy and COP. By looking for the right stuff, we will be paid, achieve a successful survey and secure a win in the VBP world.
Axxess Home Health, a cloud-based home health software, includes HIPAA-compliant documentation capabilities on all devices, even without internet access.
