
The Home Health Consumer Assessment of Healthcare Providers and Systems (HHCAHPS) patient engagement survey impacts the bottom line of home health agencies substantially, by attracting referral sources and value-based reimbursement. It is imperative for organizations to understand the HHCAHPS survey, and work on improving each measure to maximize long-term growth and sustainability.
Discussing Pain – Question 10
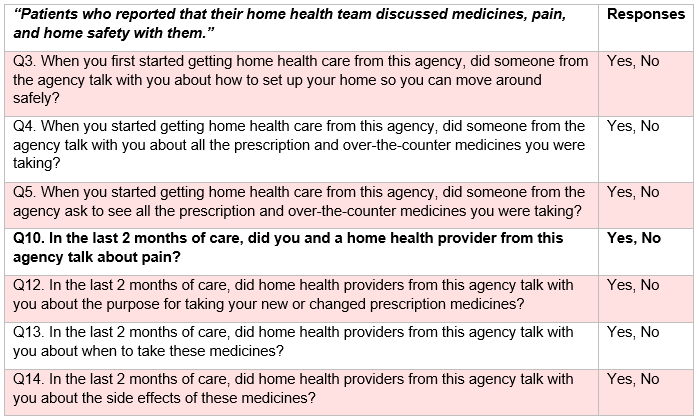
Question 10 is one of seven questions included in the Home Health CAHPS survey Specific Care Issues domain, designed to assess how effectively healthcare providers discuss medicines, pain, and home safety with patients.
Specific Care Issues
Successfully managing patients’ pain begins with effective pain assessment. Comprehensive pain assessment includes maintaining thorough documentation of details related to pain, including the below examples outlined in a recent study on pain management:
Pain Assessment
- Pain intensity (at present time, on average, lowest level of pain and most severe level of pain)
- Pain characteristics (location, frequency, factors that exacerbate pain, factors that relieve pain)
- Level of interference with daily activities (physical/psychological/social daily functioning)
- Pain behavior (facial expressions, vocalizations, body language and movements, etc.)
- Pain treatment (pharmacological and nonpharmacological therapies)
- Coping style (praying, hoping, catastrophizing, distraction from pain, etc.)
- Sensory and cognitive assessment (hearing, sight, cognitive capacity and orientation)
- Proxy reporting (accounts from family member, caregiver, or healthcare professional as applicable)
Agencies should incorporate pain assessment resources into routine procedures as needed to ensure pain assessments lead to successful development of productive treatment plans. Agencies using an Electronic Health Record (EHR) system should take full advantage of the comprehensive pain assessments integrated in visit notes, especially notes completed at Start of Care and transitional times (e.g., Resumption of Care, Recertification, and Follow-Ups). An EHR system will ideally include the option to use standardized pain assessment tools within the system, which assist agencies in maintaining structure and cohesion throughout pain assessment. Examples of standardized pain assessment tools include the Numeral Rating Scale (NRS), Global Pain Scale, Wong-Baker FACES Pain Rating Scale, and Pain Assessment in Advanced Dementia (PAINAD) Scale. Home health agency leadership should work to identify a pain assessment process that is ideal for their organization and patient population.
Pain Monitoring
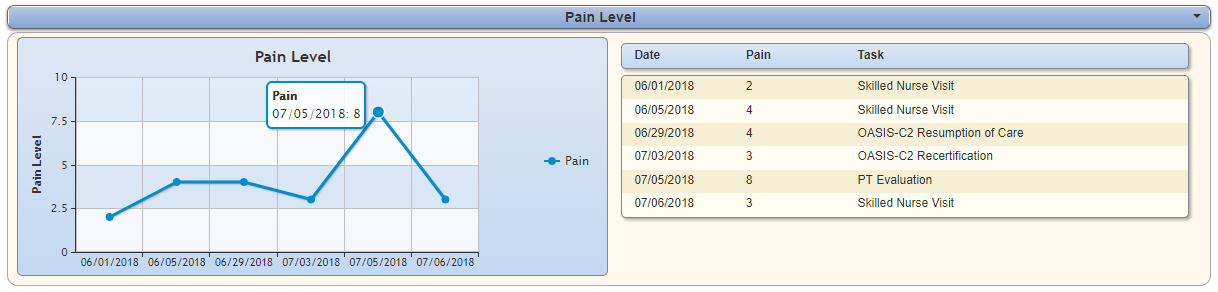
Superior EHR systems should also include a Pain Level section in each patient’s Vital Signs Chart for continuous monitoring. A Vital Signs Chart displays patient vital signs (including pain level) entered during the patient’s most recent seven visits. The chart displays in a list view and graphical format for easily reviewing trends and progress toward pain goals. Clinicians can access this resource to review the patient’s pain levels and quickly determine if adjustments are needed to better control pain.
The screenshot below shows an example of a model Pain Level section in a test patient’s Vital Signs Chart. Hovering over any point in the chart should provide a pop-up box indicating the date of the visit and pain level recorded. If the patient’s pain level is continually increasing or remaining stagnant across multiple visits, the clinician should make the appropriate adjustments to improve pain management.
Pain Education and Communication
Many factors contributing to the undertreatment of pain can be addressed through patient education and effective patient-provider discussions related to pain, as well as systematic staff training on pain assessment and management procedures. Healthcare providers should be trained exhaustively on communication best practices to ensure patients understand the importance of discussing pain and notifying providers when they experience pain. Provider responses to reported pain should involve active listening and empathetic communication techniques to encourage constructive, ongoing discussion and assure patients that their voices are heard.
Agencies can supply talking points to help guide healthcare providers through the process of educating patients and discussing pain effectively. A basic framework of workable talking points is provided below:
Talking Points for Discussing Pain with Patients
- “Please always tell us if you experience pain. Communicating your pain is necessary to ensure your safety and keep you as comfortable as possible.”
- “Managing and controlling your pain is very important because it impacts the overall effectiveness of your treatment.”
- “Some people are hesitant to use certain medications because of the associated side effects. Medication side effects can be successfully managed, and we will monitor you closely to ensure any medications used in your treatment are therapeutic and safe.” (Be sure not to assume that the patient already knows medical terms, such as opioids, analgesics, and NSAIDS. Explain healthcare terminology as needed when discussing pain management.)
- “Your opinions are valued, and your input is helpful as we work together to coordinate the best possible treatment plan for you.”
For additional talking points, the following handbook provides valuable information on care improvement through pain management: Patient Safety and Quality: An Evidence-Based Handbook for Nurses (page 478).
Check our blogs for the series on improving your agency’s HHCAHPS scores by systematically reviewing each of the HHCAHPS questions and sharing opportunities for improvement.
