The Home Health Consumer Assessment of Healthcare Providers and Systems (HHCAHPS) patient engagement survey impacts the bottom line of home health agencies substantially, by attracting referral sources, value-based reimbursement, and payment under the Patient-Driven Groupings Model (PDGM). It is imperative for organizations to understand the HHCAHPS survey, and work on improving each measure to maximize long-term growth and sustainability.
Overall Rating of Care Provided– Question 20
Question 20 is the first of two Global Rating Measures included in the Home Health CAHPS survey.
Overall Rating of Care Provided
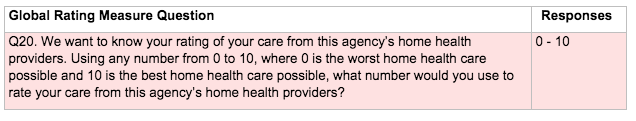
This question measures the patient’s overall perception of the care provided on a quantitative scale of 0 to 10. When reported publicly, this question reflects the percentage of patients who answered with a rating of 9 or 10, as shown in the following example: 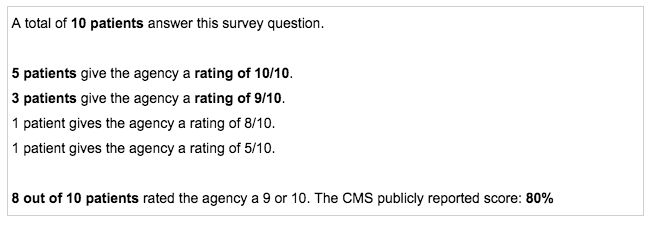
Patients who rate their agency any number from 0 to 8 lower the publicly reported percentage, so it is imperative that agencies constantly strive to provide the best possible patient experience to achieve optimal HHCAHPS survey performance and promote positive patient outcomes.
Earlier installments in our HHCAHPS improvement blog series examine each preceding survey question individually and explore opportunities for targeted improvement with embedded resources specific to each question. Additionally, the Axxess Help Center provides a content listing of these articles, sectioned by HHCAHPS survey composite, so locating resources to target specific areas of the survey is easy. Optimizing performance in all HHCAHPS survey areas will enhance global ratings. Most critically, however, healthcare organizations must fundamentally acknowledge patient experience as the key differentiator in how healthcare systems are perceived. Implementing efforts to optimize individual HHCAHPS survey questions is a fragmented approach without a basis grounded in patient experience and a commitment to delivering patient-centered care.
The Beryl Institute, an international community of practice dedicated to improving the patient experience, identifies eight guiding principles for achieving excellence in patient experience. Below the guiding principles are outlined with excerpts detailing each principle and demonstrating application in post-acute settings.
Guiding Principles for Patient Experience Excellence
1. Identify and support accountable leadership with committed time and focused intent to shape and guide experience strategy.
Improving the patient experience requires solid, ongoing staff training organized and led by agency leadership. Staff training should follow a prearranged action plan, so all efforts contribute to the organization’s common goals for improving patient experience.
2. Establish and reinforce a strong, vibrant and positive organizational culture and all it comprises.
The culture of an organization has a direct impact on the experiences of its patrons. Agency leadership should keep a constant pulse on the health of the organizational culture throughout all operations, including patient experience initiatives. Reinforce constructive values by ensuring staff members understand the meaning behind improvement efforts and the individual role each team member plays in achieving organizational goals.
3. Develop a formal definition for what experience is to your organization.
The Beryl Institute defines patient experience as, “the sum of all interactions, shaped by an organization’s culture, that influence patient perceptions across the continuum of care.” Patient experience definitions should reflect an organization’s specific goals, concentrations and values, and the unique population it serves.
4. Implement a defined process for continuous patient and family input and engagement.
Patient and family engagement are essential and should be integrated throughout an agency’s strategy for improving patient experience. The Institute for Patient- And Family-Centered Care (IPFCC) encourages healthcare systems to recognize families as partners– not visitors. The Better Together campaign, run by IPFCC, provides resources for healthcare professionals and agencies to view, customize, download, print, and distribute to engage families in patient care and integrate collaboration and teamwork throughout the strategy to improve patient experience.
5. Engage all voices in driving comprehensive, systemic and lasting solutions.
Healthcare providers and recipients (patients/families) should sustain collaborative partnerships in which all sides are empowered to exchange ideas and information, contribute to conversations that influence healthcare decisions, and work collectively toward treatment goals. Agency processes should ensure all voices are heard and reinforce the importance of collaboration.
6. Look beyond clinical experience of care to all interactions and touch points.
An article published by Modern Medicine Network outlines ten tips to provide “great customer service” to patients and demonstrates the importance of attending to interactions outside of traditional clinical contact. Examples include remembering patient names, expressing appreciation for and gratitude toward patients, and exceeding patients’ expectations by continuously ensuring care delivery and all its moving pieces are easy and pleasant.
7. Focus on alignment across all segments of the continuum and the spaces in between.
Aligning all aspects of healthcare relies on efficient, well-organized processes. As much as possible, healthcare organizations and professionals should optimize the flow of processes with technology, innovation and collaboration.
8. Encompass both a focus on healing and a commitment to well-being.
The Institute for Healthcare Improvement (IHI) recognizes June 6, 2019 as What Matters to You? (WMTY) Day, which promotes and supports more meaningful conversations between patients and providers, by encouraging practitioners to ask their patients what matters.
An article written by Susan Edgman-Levitan, PA, co-author of the original publication prompting WMTY (which discussed shared decision-making in healthcare) outlines ways to integrate WMTY concepts into every day, and demonstrates how discussing what matters to patients enables more efficient, more effective care delivery. “[When clinicians] learn how to talk with patients about what is most important to them up front, it saves time. They get more useful information that helps them make the right diagnosis and develop the most appropriate care plan. It also helps develop a partnership that leads to better outcomes.”
The “what matters” concept represents the patient experience movement at its core, reconnecting the healthcare industry to the importance of humanness in healthcare.
Check our blogs for the full series on improving your agency’s HHCAHPS scores by systematically reviewing each of the HHCAHPS questions and sharing opportunities for improvement.