Medicare episodes beginning on or after January 1, 2020, must follow the Patient-Driven Groupings Model (PDGM).
The following features enable organizations to stay compliant and successfully manage billing workflow changes under PDGM, including 30-day billing periods, no-pay RAP claims, new LUPA thresholds, and pre-claim review updates.
Under PDGM, claims will automatically generate in two 30-day billing periods per episode, instead of the previously generated 60-day billing periods under PPS.
Days 1-30 will comprise the first billing period. Days 31-60 will comprise the second billing period.
Each billing period will be assigned a RAP and a Final claim.
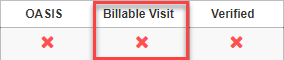
OASIS for the first 30-day RAP will consider one of the following:
OASIS for the second 30-day RAP will consider one of the following:
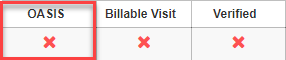
Billable Visit
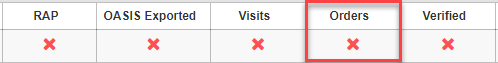
RAP verification confirms that the RAP claim associated with the Final claim is not in Created, Rejected or Denied status.
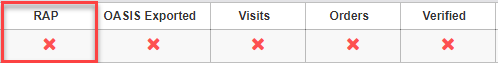
OASIS Exported for the first 30-day RAP will consider one of the following:
OASIS Exported for the second 30-day RAP will consider one of the following:
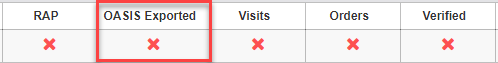
Visits confirm that all visits within the 30-day billing period are complete/approved by QA. Visits within the episode but outside of the current billing period are not included.
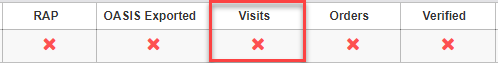
Orders for the first 30-day period will consider the following:
Orders for the second 30-day period will consider the following:
PDGM introduces three new occurrence codes to be reported on Final claims:
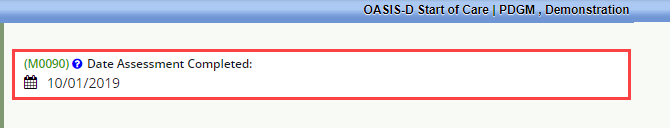
Occurrence code 50 – Assessment Date
This required code reports the assessment completion date (M0090).
Occurrence code 61 – Hospital Discharge Date
This non-required code reports the discharge date of an inpatient hospital admission that ended within 14 days of the billing period From date. This code classifies the 30-day period as Institutional.
Occurrence code 62 – Other Institutional Discharge Date
This non-required code is reported if applicable on admission claims only. It reports discharge from a SNF, LTCH, IRF, or IPF within 14 days of the billing period From date. The claim From date and Admission date must match for the period to be classified as Institutional.
All new occurrence codes will automatically be completed based on data entered in the OASIS.
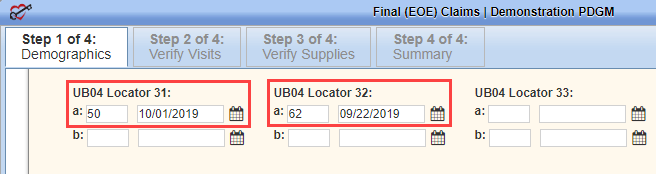
Occurrence codes 61 and 62 will populate in the UB04 Locator 31 field for the billing period’s Final claim.
Data generates based on the appropriate OASIS assessment’s M1000 and M1005 items, depending on the Discharge Date selected.
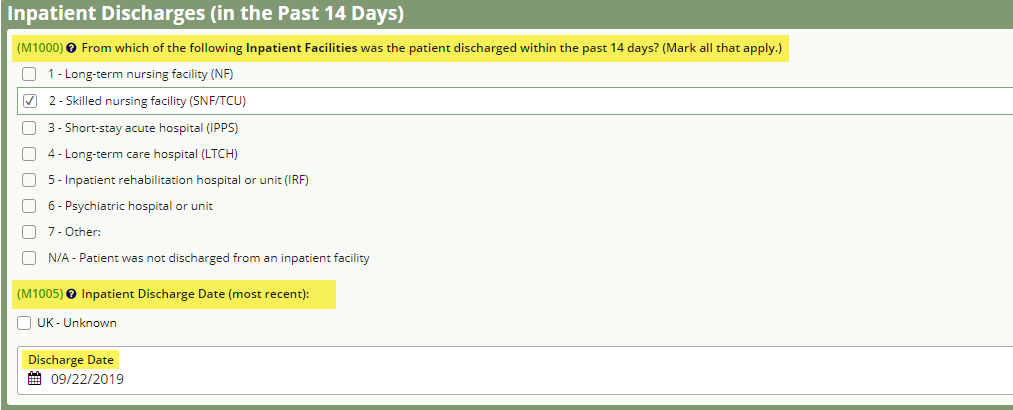
The OASIS $ icon contains the first or second billing period value.
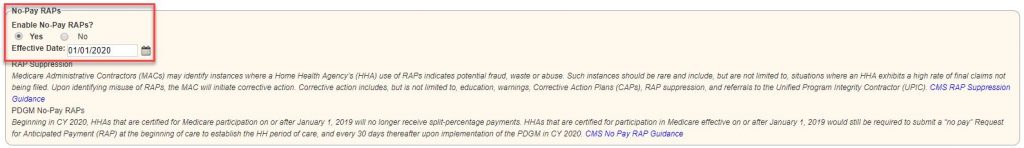
Claim values are split based on the agency’s certification dates:
.
Agencies certified on or after January 1, 2019, are encouraged to enable the No-Pay RAP feature in the Medicare payer setup section of the system to ensure claim amounts are distributed correctly.
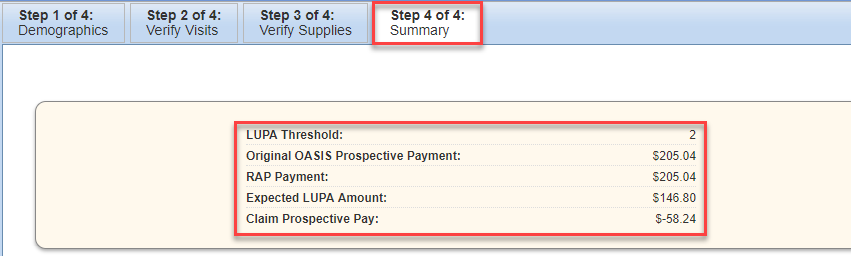
Each billing period will be assigned a LUPA threshold from the corresponding OASIS assessment.
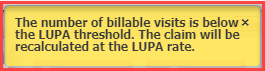
If the number of billable visits within the 30-day billing period is under the LUPA threshold count, the claim is considered a LUPA. LUPAs will undergo a LUPA recalculation to determine the claim amount. The LUPA recalculation will take place after verifying Step 2 of 4 Verify Visits of the Final claim.
When the biller verifies a past Step 2 of 4 Verify Visits on a LUPA claim, a yellow warning message notifies the user that the number of billable visits is below the LUPA threshold count.
On Step 4 of 4 Summary, the recalculated LUPA data will be available for review.
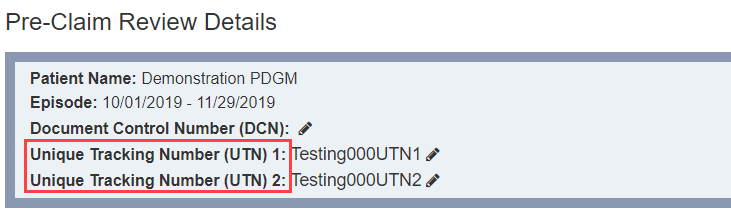
For Medicare episodes beginning on or after January 1, Medicare will assign a Unique Tracking Number (UTN) to each billing period.
Medicare will still allow pre-claim review documents to be submitted for the entire 60-day episode and will return UTNs for each billing period.
Enter the first 30-day UTN in the Unique Tracking Number (UTN) 1 field and the second 30-day UTN in the Unique Tracking Number (UTN) 2 field.
For episodes beginning on or before December 31, 2019, enter only one UTN for the episode in the Unique Tracking Number (UTN) 1 field.
Updated on 1/01/2020