In a new MLN Matters article,1 Medicare notified home health agencies that payment codes on home health claims will be matched against patient assessments. Medicare also stated that payments will be denied in the future when the Outcome and Assessment Information Set (OASIS) is not submitted before billing Final or End of Episode (EOE) claims.
When an agency enters OASIS data into a software system, the OASIS answers generate a Health Insurance Prospective Payment System (HIPPS) code which translates into the episode payment rate. Previously, the transmission of OASIS assessment data and submission of claims were completely separate processes. The intermediary, who processes payments for home care, did not have access to the quality data within the OASIS and, as a result, could not validate the HIPPS code against the associated OASIS assessment. However, since the addition of a file exchange interface, intermediaries will be able to ensure that the HIPPS generated from the assessment and the HIPPS that is billed match.
For HHPPS claims received on or after April 1, 2015, Medicare will validate the submitted HIPPS code against the OASIS-calculated HIPPS code present in the Quality Information Evaluation System (QIES).2 If the codes do not match, the OASIS generated HIPPS code will be used for payment. If the HIPPS code matches, or if an OASIS assessment corresponding to the claim is not found, the claim will process normally at this time. If the matching process changes the HIPPS code used for payment, special coding on the remittance advice will notify the agency. Agencies do not need to do anything differently in their billing process due to this change. HHPPS claims will be suspended temporarily during processing to allow for the file exchange between Fiscal Intermediary Shared System (FISS) and Quality Information Evaluation System (QIES). The claims will be suspended with FISS reason code 37071 in status/locations SMFRX0-SMFRX4. This will occur during the 14 day payment period and “should not delay payments to HHAs.”3
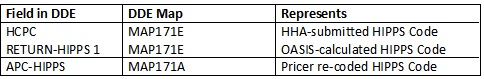
The FISS will display a new field in Direct Data Entry (DDE) that will contain the OASIS-calculated HIPPS code. The field will be named ’RETURN-HIPPS1’. When the OASIS calculated HIPPS code is used for payment, the code in this ’RETURN-HIPPS1’ field will match the code on the electronic remittance advice.
Should Medicare systems re-code the OASIS calculated HIPPS due to different therapy services provided than projected, or in cases where the episode timing (early or later) is incorrect, the re-coded HIPPS code will be used for payment and will continue to be recorded in the APC-HIPPS field. Agency billers will be able to deduce this because there will be three HIPPS codes in DDE:
Remember, the submission of OASIS is a Condition of Participation for all home health episodes as a condition of payment. If the OASIS is NOT FOUND during medical review of a claim, the claim is denied. CMS plans to use the claims matching process to enforce this Conditions of Participation (CoP) as soon as available. At that time, Medicare will deny claims on episodes in which no OASIS data is found in QIES. CMS will provide further notification as to when this implementation date will be. Agencies should ensure internal processes are in place to ensure that OASIS data is submitted before the claim (meaning final bill or EOE) is submitted to avoid future payment denials.