How can a consumer identify which home health agencies provide the best care? This is one of the reasons the Centers for Medicare & Medicaid Services (CMS) created the Home Health Compare (HHC) website for all Medicare-certified home health agencies (HHAs). This website provides information on demographics and services provided, quality of care, and patient experience ratings, utilizing a uniform set of measures to help consumers compare them. The star ratings will be added to the HHC website mid-July 2015 and updated quarterly. As an agency owner, it is important that you are familiar with the fundamentals of HHC and consider how it may impact your organization.
The 2009 passage of the Affordable Care Act (ACA) required CMS to create an easily understood, transparent public reporting of quality of care information. In response to this request, they created a 5-star rating system for use in all their programs (Nursing Homes, Dialysis Facilities, Physician Compare, Medicare Plan, which were previously implemented, and now home health). The HHC Star Ratings are calculated with a subset of publically reported home health quality measures, and are tailored to meet the needs of consumers by being displayed in a format that is easy to view and understand. CMS conducted three Open Door Forums to introduce and expand on the HHC Star Rating system. The forums garnered comments on concerns around consumers appropriately understanding and interpreting the star rating.
In order for an HHA to receive an overall HHC Star Rating, they must have been certified by CMS for at least six months, with data reported on at least five of the nine contributing quality measures during the reporting period. In order for data to be reported for a specific quality measure, the HHA must have 20 or more episodes of care with information on that measure for the previous 12-month period. Consistent with the standard applied under the home health quality reporting requirements, i.e., Pay-for-Reporting (P4R), an episode of care is defined as follows: “the submission of a matching pair of OASIS assessments (i.e., admission and discharge assessment) for a patient that has been admitted and discharged during the reporting period.”[1]
The nine measures selected for inclusion in the HHC Star Ratings calculation are based on the following criteria:[2]
- The measure applies to a substantial proportion of home health patients, so that it can be reported for a majority of home health agencies.
- The measure shows a reasonable amount of variation among home health agencies, and it is possible for a home health agency to show improvement in performance (i.e., the measure cannot be ‘topped out’).
- The measure has high ‘face validity’ (can be taken at face value) and clinical relevance.
- The measure cannot be susceptible to random variation over time.
The measures meeting the selected criteria are:
Process Measures
- Timely initiation of care
- Drug education on all medications provided to patient/caregiver
- Influenza immunization received for current flu season
Outcome Measures
- Improvement in ambulation
- Improvement in bed transferring
- Improvement in bathing
- Improvement in pain interfering with activity
- Improvement in dyspnea
- Acute care hospitalization
Patient Experience Measures
These measures will be added by CMS later in 2015.
HHC Star Rating Calculation
The HHC Star Rating calculation is a detailed, multi-step process; however, below is the abbreviated version.[3]
- First, HHAs are ranked according to their score individually on each of the nine quality measures.
- Second, for each measure the scores across all HHAs are divided into ten categories by ranking such that approximately 10 percent of agencies fall into each category.
- Third, the HHA’s preliminary star rating for each measure is then adjusted according to a statistical significance test of the difference between the agency’s quality measure score and the national median for that quality measure.
- Finally, for each HHA, the adjusted individual star ratings are averaged across all of the nine measures and assigned a star value based on a scale from one to five stars, to obtain an overall star rating for the agency.
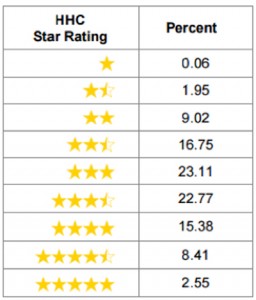
The HHC Star ratings methodology was applied to the HHC data for calendar year 2013 and only 2.5 percent of agencies had a rating of 5 stars, with the majority of agencies (62.63 percent) distributed across 2.5 – 3.5 star ratings. Based on the data provided, it appears achieving 5 stars will be challenging although not impossible; and agencies will need to focus on improving their scores on the nine measures and their CAHPS results to achieve a 5 star-rating.
Figure 1 — Distribution of Overall HHC Star Ratings, CY 2013
The HHC 5-star rating is another initiative that serves as a marker for the transition in healthcare reimbursement from fee-for-service to value-based care. It highlights the need for agencies to better understand their quality measures as well as how they are generated and can be improved. The HH-CAHPS measures should be considered an important component for not only how patients rate their experience with your agency and shared with the general public, but will soon be added to the 5-star report.
Each agency is able to receive a preview report of their 5-star report in CASPER, and your CAHPS vendor may provide a complimentary copy. If you are not currently at a 5-star rating, remember your current rating is a starting point and you can improve your rating as you improve your understanding of the report and take corrective action to improve your processes and see positive improvement. As an agency owner, you would be wise to embrace and leverage the HHC 5-star rating to ensure consumers shopping for home health services find the exceptional quality and service you provide.
Axxess offers a complimentary 5-star preview report for customers subscribed to its CAHPS services and will continue building and providing tools such as the 5-star report to empower customers for success and excellence in patient care.
[1] http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HomeHealthQualityInits/Downloads/HHC-Star-Ratings-FAQs-updated-2-27-15.pdf
[2] http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HomeHealthQualityInits/Downloads/Home-Health-Star-Ratings-Methodology-updated-3-16-15.pdf
[3] http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HomeHealthQualityInits/Downloads/Home-Health-Star-Ratings-Methodology-updated-3-16-15.pdf
[4] http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HomeHealthQualityInits/Downloads/Star-Ratings-Methodology-updated-3-16-15.pdf