Centers for Medicare and Medicaid Services (CMS) recently announced that home health agencies (HHAs) operating in areas affected by Hurricane Harvey will allow agency staff to focus on patient care while in the midst of recovery.
On August 31, 2017, CMS announced that blanket waivers had been issued for several provider types, including HHAs, in Texas counties and Louisiana parishes declared disaster areas by the Federal Emergency Management Agency (FEMA).
Waivers to HHQRP
The waivers include an exception to Home Health Quality Reporting Program (HHQRP) requirements, or "pay for performance," for the second and third quarters of 2017. Other waivers will delay or suspend re-certification and revisit surveys, allowing additional time for providers to submit plans of correction among other helps.
Current HHQRP regulations, including 484.20(c)(1), require HHAs to achieve at least a 90 percent compliance rate when exporting matching OASIS assessments to create a quality episode within the reporting period. Quality episodes begin when care is initiated and end when care ceases.
Agencies who do not meet the 90 percent quarterly compliance rate typically see a two percent reduction across the board of final claims payments. However, for agencies in declared disaster areas, this threshold has been waived for the second and third quarters of 2017. The state or impacted provider should forward provider information and waiver requests to the CMS Dallas Regional Office for tracking purposes (see contact information below).
Other Waivers
CMS-issued other blanket waivers that may impact HHA practices in Harvey impacted areas:
- Waiving requirements that critical access hospitals must limit the number of beds to 25, and length of stay is limited to 96 hours;
- Lifting of Part B Medicare Non-Emergency Ambulance temporary enrollment moratoria in Texas;
- Waiving the three-day prior hospitalization for coverage of a skilled nursing facility stay; the 1812(f) waiver allows nursing facility admission without the three-day hospital stay and also waives the spell of illness requirement for evacuees and others impacted by the hurricane who need skilled nursing facility care;
- Waiving of timeframe requirements for Minimum Data Set (MDS) assessments and transmission; this waiver is limited to identified impacted counties and geographical areas; and
- Loosening of Medicaid and CHIP enrollment requirements.
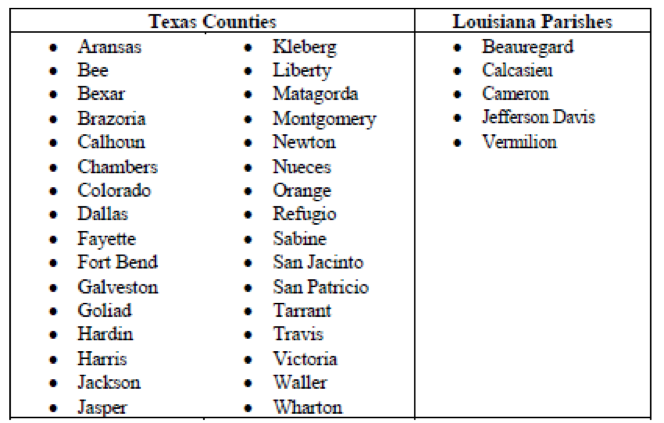
Blanket waivers apply to the following counties in Texas and Louisiana:
HHAs in these counties should be aware of the following information impacting care delivery:
- According to the Survey and Certification FAQs, Medicare-approved HHAs have the following modifications to the comprehensive assessment regulation at 42 CFR 484.55 may be made, and will support reimbursement when billing is resumed to help ensure appropriate care is provided:
- Start of Care assessment (RFA 1) may be abbreviated to include the Patient Tracking Sheet and the 24 payment items;
- Resumption of Care assessment (RFA 3) and the Recertification assessment (RFA 4) may be abbreviated to the 24 payment items;
- Discharge assessment (RFA 8 or RFA 9) and Transfer assessment (RFA 6, RFA 7) are suspended during the waiver period;
- HHAs should maintain adequate documentation to support provision of care and payment; subject to the public health emergency declarations under section 1135, for HHAs that are located in the emergency areas that serve evacuees, the SOC Assessment (RFA 1) may be abbreviated to include the Patient Tracking Sheet and the payment items;
- Abbreviated assessment does not have to meet the five-day completion date or the seven-day lock date;
- OASIS transmission requirements at 42 CFR 484.20 are suspended for those Medicare approved HHAs that are serving qualified home health patients/evacuees in the affected areas;
- Agencies are expected to use this policy only as needed, and to return to business as usual as soon as possible.
- Instructions for how to handle situations where documentation to support payment has been lost or destroyed can be found in CMS' Program Integrity Internet Only Manual in Publication 100-08, Chapter 3, §3.8, "Administrative Relief from MR During a Disaster." A note should be entered and dated in the medical record that the documentation was destroyed in the hurricane. This will include medical records for ADRs, CERTs, RACs, etc.
- Face to Face requirements, which are a condition of payment, cannot be waived under Section 1135 of the Social Security Act. If conditions related to the emergency cause a provider to expect to be unable to meet the face to face encounter timeframes, that provider should contact the CMS Regional Office to allow for tracking and completion of this encounter as soon as conditions allow.
Non-Waiver Facts
Other important information, not tied to blanket waiver programs, that HHAs need to know include:
- CMS will advise Medicare Administrative Contractors (MACs) to pay claims for beneficiaries who have been displaced due to disasters, and the MAC will work with agencies that have transferred or received patients due to the disaster or emergency. However, normal HHPPS procedures will apply, including application of Partial Episode Payment (PEP).
- Under the temporary and extraordinary circumstance of a declared emergency or disaster, place of residence can include services provided at temporary locations like a family member's home, shelter, community facility, church or hotel. A hospital, SNF or nursing facility would not be considered a temporary residence.
- For HHAs impacted, CMS is instructing the Regional Home Health Intermediaries (RHHIs) and MACs to temporarily cease and to automatically cancel the RAP for episodes that have already begun.
- HHAs should report condition under code 47, which indicates transfer from another HHA, on their RAPS for patients who were displaced by a declared emergency. This will ensure that Medicare systems do not reject their RAP due to an overlapping episode at the prior HHA. No other special indicators are needed on these RAPs.
- A Medicare-approved HHA that is able to provide home health services beyond its current geographic service area may do so on a temporary basis during the emergency period, provided that the HHA is in full compliance with state and local law, if the HHA is able to ensure that staff is competent and able to provide appropriate care, and that the purpose of the expansion is to provide care to the patients affected by the emergency. This means beneficiaries who have been receiving home health services and cannot obtain emergency-related treatment during the emergency (such as medication, vaccination, etc.) from HHAs within their service area can be seen by out-of-area HHAs.
Additional waivers are being considered and agencies in areas across the US who are impacted by hurricane damage should monitor for changes at the Hurricane Emergency website, under the "Administrative Actions" section of the page found.
Questions from providers can be sent to the Dallas Regional Office (RO) at RODALDSC@cms.hhs.gov or providers may also call their MAC for additional clarity or questions.
Additional Resources:
MLN Matters SE17020 regarding Hurricane Harvey and Disaster Related Claims, including disaster waiver program Q&A links.
Additional information regarding waiver programs for Hurricane Harvey.
For more information on home health quality reporting and quality episodes.